UCD Research - July 2023
Retrospective study on canine MUO
UCD researchers, including Monica Augusto, senior academic staff, a small animal intern and a final year veterinary medicine student have embarked on a study of canine meningoencephalomyelitis of unknown origin (MUO)
In association with

Monica Augusto
Assistant professor in small animal medicine, Section of Small Animal Clinical Studies, UCD
The team aims to investigate the typical clinical presentation, clinicopathological and imaging findings, potential risk factors and outcome of dogs diagnosed with MUO at the University College Dublin (UCD) Veterinary Hospital over the past ten years.
Meningoencephalomyelitis of unknown origin (MUO)
Meningoencephalomyelitis of unknown origin (MUO) is a heterogeneous group of central nervous system (CNS) inflammatory diseases and likely the most common non-infectious meningoencephalitis diagnosed in dogs. It is a broad term that includes granulomatous meningoencephalomyelitis (GME), necrotising meningoencephalitis (NME), greyhound meningoencephalitis and necrotising leukoencephalitis (NLE)3. Clinical presentation varies from acute rapidly developing signs to slow progressive neurological decline over weeks to sometimes months, and prognosis is also variable, possibly dependent on the histopathological MUO subtype that is rarely confirmed ante-mortem3. There is established breed predisposition, especially in small and toy dogs, so a genetic cause has been suspected to contribute to the development of MUO. However, a genetic risk loci has only been identified in Pugs and Maltese dogs8. For most dogs an underlying aetiology is usually not identified, and, therefore, MUO is presumed to be a primary immune-mediated or idiopathic disease process, with also an unknown pathophysiology5. Neurological signs are often multifocal or diffuse, and may include altered mentation, proprioceptive or cranial nerve deficits, seizures, acute onset of blindness, spinal pain, and vestibular and cerebellar signs, as well as vague systemic signs like anorexia and, occasionally, pyrexia due to CNS inflammation4.
The presumptive diagnosis of MUO depends on exclusion of other neurological conditions along with consistent findings on magnetic resonance imaging (MRI) of the brain and/or spine and cerebrospinal fluid (CSF) analysis. The diagnosis of MUO has increased in frequency over the past few decades, either because of a real increase in prevalence or due to increased awareness of the disease and the popularity of certain dog breeds5.
Dogs diagnosed with MUO are treated with immunosuppressive doses of glucocorticoids (often prednisolone) frequently in combination with other immunosuppressive medications such as cytosine arabinoside4,6.7,9, mycophenolate2,10, and cyclosporine1,3. Response to treatment is based on improvement or resolution of neurological signs, and occasionally repeated CSF analysis3-4. Glucocorticoids are the first line of therapy across all treatment recommendations, but the ideal protocol remains unclear in terms of drug choice, route (e.g., subcutaneous vs. intravenous infusion of cytosine) and even frequency of administration.
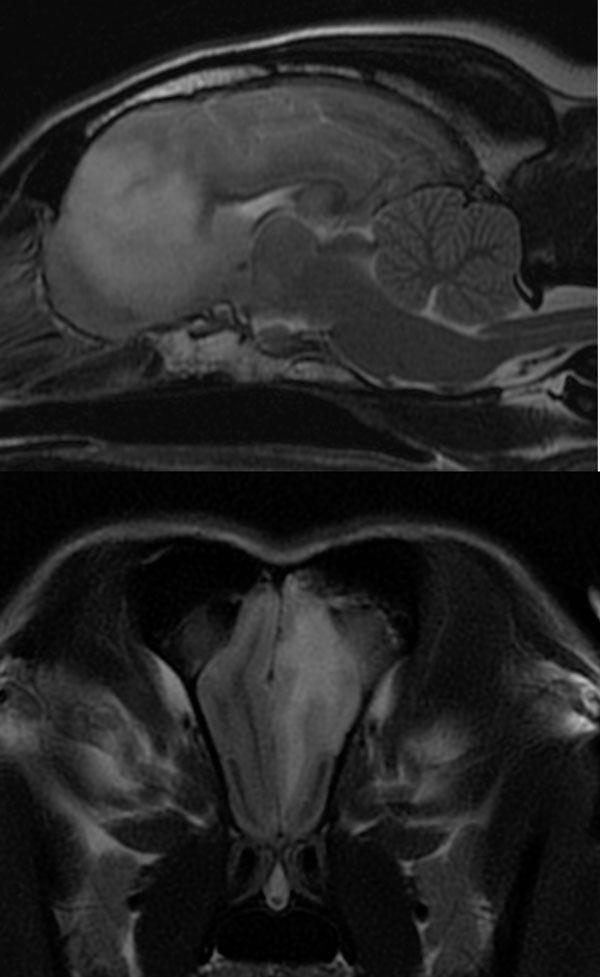
Sagittal (A) and transverse (B) T2W images of an eight-year-old female neutered Beagle diagnosed with MUO. Note the diffuse left olfactory and ventromedial aspect of the left frontal lobe hyperintensity affecting predominantly the white matter tracts on the T2W images. Image courtesy of Diagnostic Imaging Service at UCD Veterinary Hospital.
Comparative aspect to human medicine
Non-infectious (immune-mediated) meningoencephalomyelitis is common in humans and most widely apparent in the high prevalence of multiple sclerosis (MS). The clinical presentation of primary progressive MS is similar to those of MUO in dogs5. Given the extensive research into the pathogenesis of MS, and new diagnostic and therapeutic strategies, significant advances in MUO might also be seen in the near future.
Objectives and methodology
This project is a large retrospective study looking at the epidemiology, clinical presentation, diagnostic imaging findings and clinicopathological results of dogs diagnosed with MUO in view of identifying possible risk factors, patterns of immune response, and treatment drug combinations that may ultimately dictate the outcome of dogs diagnosed with MUO.
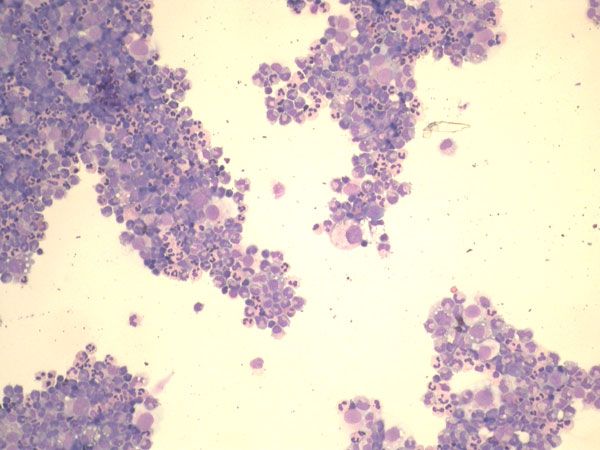
Cytology of a cytospin preparation of a cerebrospinal fluid sample (CSF) of a four-year-old female neutered Maltese dog diagnosed with MUO (200X amplification). Note the marked neutrophilic inflammation and occasional large mononuclear cells. Image courtesy of Dr Pedro Serra Dip. ACVP.
-
Adamo PF, Rylander H, Adams WM. Ciclosporin use in multi-drug therapy for meningoencephalomyelitis of unknown aetiology in dogs. J Small Anim Pract. 2007 Sep;48(9):486-96.
-
Barnoon I, Shamir MH, Aroch I, Bdolah-Abram T, Srugo I, Konstantin L, et al. Retrospective evaluation of combined mycophenolate mofetil and prednisone treatment for meningoencephalomyelitis of unknown etiology in dogs: 25 cases (2005– 2011). J Vet Emerg Crit Care. (2016) 26:116–24
-
Coates JR, Jeffery ND. Perspectives on meningoencephalomyelitis of unknown origin. Vet Clin North Am Small Anim Pract. 2014 Nov;44(6):1157-85.
-
Cornelis I, Van Ham L, Gielen I, De Decker S, Bhatti SFM. Clinical presentation, diagnostic findings, prognostic factors, treatment and outcome in dogs with meningoencephalomyelitis of unknown origin: A review. Vet J. 2019 Feb;244:37-44.
-
Jeffery N, Granger N. New insights into the treatment of meningoencephalomyelitis of unknown origin since 2009: A review of 671 cases. Front Vet Sci. 2023 Mar 15;10:1114798.
-
Lowrie M, Smith PM, Garosi L. Meningoencephalitis of unknown origin: investigation of prognostic factors and outcome using a standard treatment protocol. Vet Rec. 2013 May 18;172(20):527.
-
Lowrie M, Thomson S, Smith P, Garosi L. Effect of a constant rate infusion of cytosine arabinoside on mortality in dogs with meningoencephalitis of unknown origin. Vet J. 2016 Jul;213:1-5.
-
Schrauwen I, Barber RM, Schatzberg SJ, Siniard AL, Corneveaux JJ, Porter BF, Vernau KM, Keesler RI, Matiasek K, Flegel T, Miller AD, Southard T, Mariani CL, Johnson GC, Huentelman MJ. Identification of novel genetic risk loci in Maltese dogs with necrotizing meningoencephalitis and evidence of a shared genetic risk across toy dog breeds. PLoS One. 2014 Nov 13;9(11):e112755.
-
Stee K, Broeckx BJG, Targett M, Gomes SA, Lowrie M. Cytosine arabinoside constant rate infusion without subsequent subcutaneous injections for the treatment of dogs with meningoencephalomyelitis of unknown origin. Vet Rec. 2020 Nov 28;187(11):e98.
-
Song JH, Yu DH, Lee HC, Hwang TS, Kim YJ, An SJ, et al. Evaluation of treatment with a combination of mycophenolate mofetil and prednisolone in dogs with meningoencephalomyelitis of unknown etiology: a retrospective study of 86 cases (2009–2017). BMC Vet Res. (2020) 16:192
In association with

Monica Augusto
Assistant professor in small animal medicine, Section of Small Animal Clinical Studies, UCD