Extracorporeal shockwave therapy
Dr Siobhan Menzies BVM&S CCRP GPCert(WVA&CPM) MRCVS discusses the history of extracorporeal shockwave therapy (ESWT) and the science behind it. The differences between radial and focused shockwave are explained. The clinical indications, contraindications and practicalities of applying this therapy in companion animals are highlighted
In the 1970s, shockwaves were used to treat kidney stones in a process known as lithotripsy. The high energy focused ultrasonic waves were used to break kidney stones into smaller pieces that could then be passed. Assessment of side effects of the therapy discovered that fracture healing was enhanced and over the next decades the use of shockwaves to treat non union fractures, tendinopathies and plantar fasciitis in people was developed. Further research in the equine population followed and, more recently, use in small animals for osteoarthritis and tendinopathies has increased. During subsequent research a dose-related effect was noticed with low dosages stimulating regeneration but higher dosages causing destruction.
What are shockwaves?
Shockwaves are basically high energy acoustic compression waves which are produced after a rapid rise in pressure is followed by a short negative pressure. Another way of thinking of them is as a “controlled” explosion. Examples are thunder following lightning and a sonic boom from a jet.
Shockwaves travel through air, water, body fluids, soft tissue and bone. They release energy when they reach a tissue density interface e.g., tendon bone junction. This energy can have various biological effects in the body.
Energy flux density (EFD), measured in mJ/mm2, is the parameter used to compare shockwave treatments. EFD indicates that the shockwave energy ‘flows’ through an area perpendicular to the direction of propagation.
There are two types of wave used in ESWT: focused and radial (see Figure 1).
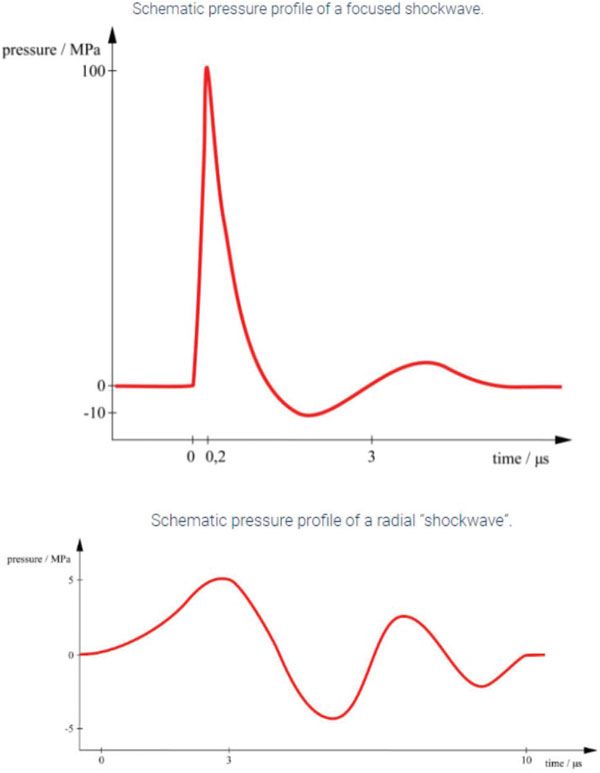
Figure 1. Schematic pressure profiles of a focused shockwave and a radial shockwave.
Focused shockwaves
The waves can be focused at a particular tissue depth and the EFD is higher at this depth than at the source. They produce an effect over a small area, deep in tissue. Focused shockwaves are produced by electrical sources creating the waves in a fluid medium.
Methods of production
Electrohydraulic - a high voltage spark gap generates a spark which triggers plasma bubbles in a fluid medium. The plasma bubbles create shockwaves which are focused by an elliptical mirror.
Electromagnetic - a coil creates current in a copper membrane which generates shockwaves in a fluid medium which are focused by an acoustic lens.
Piezoelectric - piezoelectric crystals on the inside of a hemisphere contract and expand when current is applied to them. This creates pressure waves which are concentrated on a focal point by the hemisphere.
Radial shockwaves
These are produced by ballistic or in some cases electromagnetic systems. The energy is highest at the source and decreases with distance from the source. The depth of penetration cannot be adjusted. Radial shockwave has an effect over a large but superficial area. In general, radial shockwave is a more comfortable treatment than focused shockwave. Animals will usually tolerate radial shockwave when conscious but may require sedation for focused treatments.
There is controversy over whether radial shockwaves are true shockwaves as they have slower rise times and some authors prefer the terms radial pressure waves (RPW) or extracorporeal pulse activation therapy (EPAT).
However a recent review stated that referring to focused shockwaves as high energy and referring to radial as low energy was not correct and should not be used. In addition, research does not show any evidence that one form is superior to the other.
Method of production
Ballistic compressed air accelerates a projectile in a barrel creating radial shockwaves. Kinetic energy is converted into an acoustic sound wave. The EFD is highest at the transmitter-skin interface.
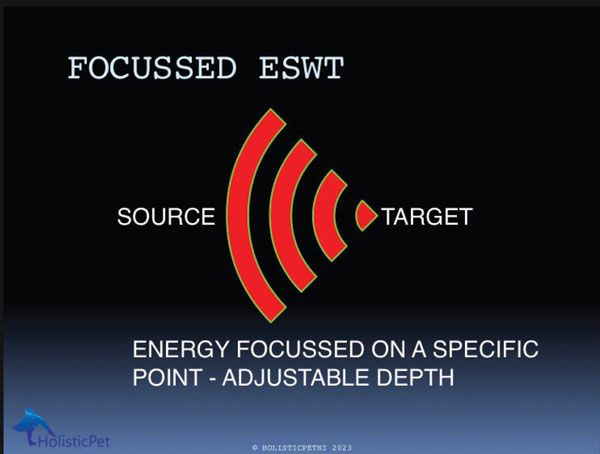
Figure 2. Focused ESWT.
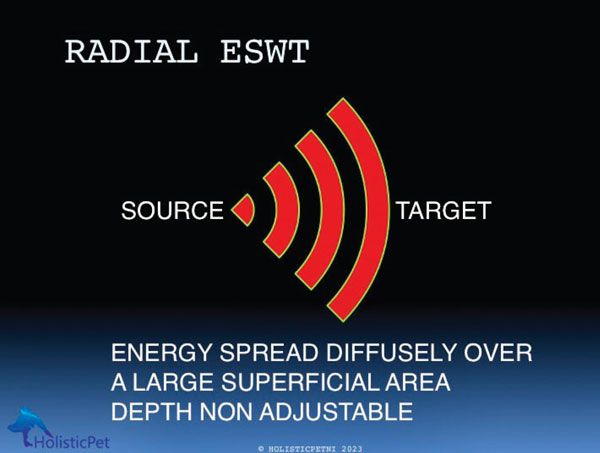
Figure 3. Radial ESWT.
ESWT parameters
These are the variables affecting shockwave treatment. Some are fixed for the device and others can be altered according to the area and condition being treated.
Peak positive and negative acoustic energy.
Total energy.
Rise time.
Frequency (Hz).
Number of pulses.
Energy per unit area/Energy flux density (EFD, mJ/mm2).
Penetration depth.
Focal area.
Number of treatments.
Anatomical site treated.
EFD - which level should you choose?
Research on ESWT on Achilles tendons showed that there was a dose-related effect. Low EFD had no effect, medium EFD caused a slight inflammatory effect while higher levels of EFD caused significant inflammation and cell necrosis. Professor Tim Watson in his book, Electrophysical Agents
(13th edition), has suggested the following as a guide:
Low < 0.08mJ/mm2
Medium 0.08-0.28 mJ/mm2
High > 0.6mJ/mm2
For radial ESWT, the pressure within the handpiece is expressed in Bar but the energy delivered will depend on this pressure plus the size, shape and type of transmitter.
Mechanotherapy
Shockwave, like therapeutic exercise, is regarded as a mechanotherapy, which has been described as “all therapeutic interventions that reduce and reverse injury to damaged tissues or promote the homeostasis of healthy tissues by mechanical means at the molecular, cellular or tissue level” (Huang, C. et al, 2013). Mechanotherapies are gaining increasing interest due to their effect on healthy and degenerating tissue.
The acoustic energy released at the tissue interface is converted into mechanical energy which has the effect of mechanical transduction, the process where agitation of cells can trigger biochemical reactions.
The processes of shockwave treatment are not yet fully understood. It is thought that the acoustic energy is released as a pressure wave when the shockwave meets a tissue interface, which is deep in tissue for focused waves but on the surface of skin/superficial tissues with radial ESWT. The positive phase of the wave has direct mechanical effects while the negative phase creates gas bubbles. Cavitation of these gas bubbles triggers a secondary shockwave. When the energy level is high, gas in the bubbles expands causing them to implode creating a destructive micro jet or ‘unstable cavitation’. This is the effect used in lithotripsy to break up kidney stones. With lower energies, the cavitation is stable and has a mechanotransduction effect on cells and the extracellular matrix (ECM).
Basically the shockwave creates short-term pain to initiate pain relief responses and inflammation to kick start the healing process, effectively a reboot of the system. Some people even regard it as a form of regenerative medicine as it stimulates the body to heal itself. Others refer to it as an inflammatory optimiser.
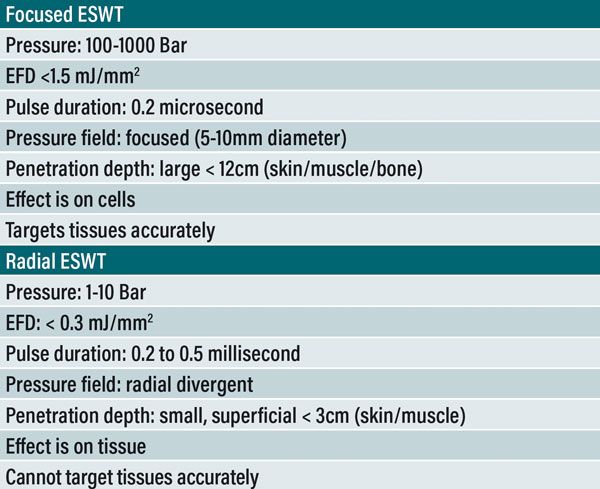
Table 1. Differences between focused and radial ESWT.
Biological effects
Tissue healing and wound repair: release of cytokines and growth factors including Nitric Oxide Synthase (NOS) which triggers neovascularisation and bone healing; transforming growth factor Beta and Insulin-like growth factor (IGF) both important for tissue healing; fibroblast growth factor 2 (FGF2) encouraging fibroblast activity and increasing collagen synthesis; vasculoendothelial growth factor (VEGF) enhancing neovascularisation; proliferating cell nuclear antigen (PCNA) for endothelial cell proliferation; activation of macrophages which are pro-inflammatory and also recruit and stimulate stem cells; increased ATP production.
Tendon healing: interleukin mediated tendon remodelling improving alignment of collagen fibres and tensile strength; reduced metalloproteinase (degrades collagen); TGFB and IGF stimulate tenocyte and collagen production; improved bone - tendon interface.
Pain relief: stimulates nociceptors reducing afferent pain gate blocking theory; reduced neurotransmitters such as Substance P and Calcitonin gene-related peptide; increased release of serotonin; enhanced descending inhibition; improved blood flow removes inflammatory mediators; down regulation of trigger points.
Bone healing: increased bone morphogenetic protein (BMP) and VEGF stimulating osteoblasts and osteogenesis plus inhibition of osteoclasts; angiogenesis and neovascularisation.
Neural effects: radial shockwave may improve cerebral blood flow, neurological function and neurogenesis.
Reduced inflammation and oedema.
Osteoarthritis: reduced inflammation and oedema; decreased activity of metalloproteinase; increased activity of chondrocytes; improved subchondral bone.
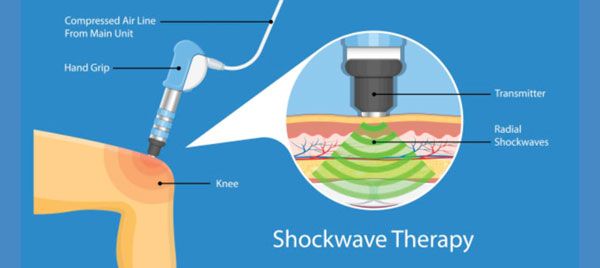
Figure 4. Shockwave therapy.
Clinical indications
Human ESWT
Shoulder tendinopathy.
Tennis elbow.
Plantar fasciitis.
Non union fractures.
Equine ESWT
Tendinopathy and desmitis in particular suspensory ligament desmopathy.
Osteoarthritis.
Non union fractures.
Small animal ESWT
Osteoarthritis.
Tendinopathies.
Wound healing.
Fracture repair.
Pain relief.
Desmitis, patellar desmitis post-TPLO potentially.
More about tendinopathies
Tendinopathies arise due to multiple small injuries that never heal, or due to chronic underuse, i.e., stress shielding. Unloading a tendon has the same effect as chronic overuse/damage. The end result of either situation is that the tendon loses tensile strength, it may be hypo or hypervascularised and there is usually evidence of new nerve endings with chronic remodelling of pain pathways as the body tries to get you to stop the activity that is causing the damage.
Tendon healing is very slow as many tendons have poor circulation. It can take up to 12 months for a tendon to heal. Wolff’s Law, developed by the German anatomist and surgeon Julius Wolff (1836–1902), states that bone in a healthy animal will adapt to the loads under which it is placed and this principle can be extended to other connective tissues including tendons. Tendon healing requires some stress but excess stress while the tendon is healing can be traumatic.
Traditional treatment for tendinopathy is to rest it and prescribe NSAIDs. Rest unloads the tendon resulting in reduced strength, so that when the patient returns to its normal activity, it injures the tendon again. In addition one of the hallmarks of tendinopathy is the lack of inflammation. Use of NSAIDs in chronic tendinopathies is therefore not clinically indicated. Tendinopathy is more correctly a degenerative process. What we need to do is to kick-start the healing process, improve the blood supply, and control the pain.
Rehabilitation of tendinopathy requires a combination of pain relief, stimulation of tissue healing, encouraging collagen fibre realignment and a controlled return to function. Above all, patience is required and the client must be informed at the start that the process will take a long time.
Stimulate healing: ESWT +/- PRP, laser, manual therapy.
Protect from reinjury: activity modification especially avoiding the problematic exercise.
Guided return to activity: therapeutic exercise including eccentric strengthening. Progressive loading of the tendon. It can take months for a tendon to heal adequately.
Contraindications and precautions of ESWT
Greater caution is necessary with focused ESWT than with radial shockwave.
Over the lung field, pregnant womb, brain, major blood vessels or nerves.
Unstable fractures.
Tumours.
Infection, e.g., discospondylitis.
Immune mediated arthritis.
Acute inflammation.
Neurological deficits.
Over metal implants.
Over open growth plates or in skeletally immature animals.
Risk of bruising is increased if ESWT is used in patients with coagulopathy or if the patient is on NSAIDs.
Avoid excess energy or number of pulses particularly close to tendons or ligaments.
Over-active bleeding, thrombophlebitis or deep vein thrombus.
In sedated patients.
Over electronic implants, e.g., pacemaker.
See also the list of contraindications here:
https://www.electrotherapy.org/contraindications-1
Practical application
Stop NSAIDs 48 hours prior to treatment due to increased risk of bleeding. To provide additional pain relief, use multimodal pain management, i.e., other meds, or combine with other modes of pain relief, e.g., TENS, massage, acupuncture, laser. May also be combined with regenerative medicine PRP or stem cells. If the shockwave causes significant pain, NSAIDs may need to be reinstated but any discomfort usually settles after 24 to 48 hours.
Clip the area, clean and wipe with alcohol.
Apply coupling medium e.g., ultrasound gel.
Lateral recumbency.
Sedation or GA is required for some focused ESWT but radial ESWT is better tolerated without sedation.
Careful anatomical application.
Select pressure (mJ/mm2 or bar).
Select frequency.
Select number of pulses.
Hold the applicator perpendicular to the skin and DO NOT TILT in focused ESWT.
Apply light pressure to maintain good contact.
Start at a low frequency (8Hz) and energy, and gradually increase after every 200 impulses.
Use highest energy tolerated for focused shockwave in unsedated animals.
Move along the line of the proximal and distal joint capsule.
Move along the muscle for myalgia or tense muscle.
Small oscillatory movements are required for localised areas, e.g., for myofascial trigger points or tendons.
Repeat once a week or fortnight for two or three treatments.
Warn owners it may take one to four weeks to see results.
Patients’ symptoms may be aggravated for a day or two.
Examples of treatment protocols
Focused shockwave
Hip joint – apply to acetabular and femoral head joint capsules. Pressure 0.13-0.15 mJ/mm2, 500-1000 shockwaves.
Elbow joint – humeral, radial and ulnar joint capsule. Pressure 0.1-0.13 mJ/mm2, 800-1000 shockwaves divided among four quadrants.
Stifle joint – femur and tibial joint capsule. 0.13-0.15 mJ/mm2, 800-1000 pulses among four quadrants.
Tendinopathies – apply to affected tendon. Pressure 0.12-0.13 mJ/mm2, 200-500 pulses.
Radial shockwave
Hip joint – lateral or ventral. Pressure 2 bar, 500-2000 shockwaves. Avoid greater trochanter.
Elbow joint – lateral and medial. Pressure 1.8 bar, 1000-2000 shockwaves divided between lateral and medial.
Stifle joint – lateral and medial. 1.5 bar, 1000-2000 shockwaves divided between lateral and medial.
Tendinopathies – apply to affected tendon. Pressure 1.7 bar, 500-800 pulses.
Side effects
Bruising/petechiation.
Swelling.
Temporary aggravation of symptoms.
Usually settle within 48 hours.
- Effect of extracorporeal shockwave therapy on elbow osteoarthritis in dogs - aaha. Available at: https://www.aaha.org/globalassets/04-practice-resources/gotopracticesolutions/resources/effect-of-extracorporeal-shock-wave-therapy-on-elbow-osteoarthritis-in-dogs.
- Alfredson, H. et al. (1998) ‘Heavy-load eccentric calf muscle training for the treatment of chronic achilles tendinosis’, The American Journal of Sports Medicine, 26(3), pp. 360–366. doi:10.1177/03635465980260030301.
- Barnes, K. et al. (2019) ‘Extracorporeal shockwave therapy improves short‐term limb use after canine tibial plateau leveling osteotomy’, Veterinary Surgery, 48(8), pp. 1382–1390. doi:10.1111/vsu.13320.
- Bockstahler, B. et al. (2019) Essential Facts of Physical Medicine, Rehabilitation and Sports Medicine in Companion Animals. 1st edn. Babenhausen: VBS GmbH.
- Cacchio, A. et al. (2006) ‘Effectiveness of radial shock-wave therapy for calcific tendinitis of the shoulder: Single-blind, randomized clinical study’, Physical Therapy, 86(5), pp. 672–682. doi:10.1093/ptj/86.5.672.
- Durant, A. and Millis, D. (2014) ‘Applications of extracorporeal shockwave in small animal rehabilitation’, Canine Rehabilitation and Physical Therapy, pp. 381–392. doi:10.1016/b978-1-4377-0309-2.00022-3.
- Fitch, G. et al. (2005) ‘The evaluation of extracorporeal shockwave therapy in naturally occurring osteoarthritis of the stifle joint in dogs’, Veterinary and Comparative Orthopaedics and Traumatology, 18(03), pp. 147–152. doi:10.1055/s-0038-1632954.
- Huang, C. et al. (2013) ‘Mechanotherapy: Revisiting physical therapy and recruiting mechanobiology for a new era in medicine’, Trends in Molecular Medicine, 19(9), pp. 555–564. doi:10.1016/j.molmed.2013.05.005.
- Ilieva, E. (2012) ‘Radial shockwave therapy in the treatment of lateral epicondylitis’, Annals of Physical and Rehabilitation Medicine, 55. doi:10.1016/j.rehab.2012.07.194.
- Millis, DVM, DACVS, CCRP, DACVSMR; M Drum, DVM, PhD, CCRP; D Whitlock, PT, DVM, CCRP, D., Drum, DVM, PhD, CCRP; D Whitlock, PT, DVM, CCRP, M. and Whitlock, PT, DVM, CCRP, D. (no date) Effect of extracorporeal shockwave therapy on elbow osteoarthritis in dogs, www.asha.org. Available at: https://www.aaha.org/globalassets/04-practice-resources/gotopracticesolutions/resources/effect-of-extracorporeal-shock-wave-therapy-on-elbow-osteoarthritis-in-dogs.pdf (Accessed: 09 July 2023).
- Van der Worp, H. et al. (2013) ‘No difference in effectiveness between focused and radial shockwave therapy for treating patellar tendinopathy: A randomized controlled trial’, Knee Surgery, Sports Traumatology, Arthroscopy, 22(9), pp. 2026–2032. doi:10.1007/s00167-013-2522-z.
- Wang, C.-J., Huang, H.-Y. and Pai, C.-H. (2002) ‘Shockwave-enhanced neovascularization at the tendon-bone junction: An experiment in dogs’, The Journal of Foot and Ankle Surgery, 41(1), pp. 16–22. doi:10.1016/s1067-2516(02)80005-9.
- Watson , T. and Nussbaum, E. (2021) Electro Physical Agents - Evidence Based Practice . 13th edn. Edinburgh London New York Philadelphia St Louis Sydney: Elsevier.
Dr Menzies graduated from the Royal (Dick) School of Veterinary Studies in 1990. She holds a CCRP (Canine Certified Rehabilitation Practitioner - a RACE-approved university qualification in canine rehabilitation) and a GP Certificate in Western Veterinary Acupuncture and Chronic Pain. In 2003, she established HolisticPet, Northern Ireland’s first veterinary pain management and rehabilitation practice. HolisticPet now offers veterinary-led pain management clinics in Northern Ireland, Kent and East Sussex. Siobhan has prepared a course on practical rehabilitation for the veterinary profession which will be available later this year via Longview CPD.
1. Which of the following statements are not correct? Choose one answer.
A. Radial shockwave is usually a more comfortable therapy than focused shockwave
B. Focused shockwave can target specific tissues
C. With radial shockwave the EFD is lowest at the transmitter-skin interface
D. Focused shockwave has a large penetration field, potentially up to 12cm
E. The EFD of radial shockwave is typically less than 0.3mJ/mm2
2. For the treatment of Achilles tendinopathy an EFD of greater than 0.28mJ/mm2 is recommended.” True or false?
A. True
B. False
3. ESWT is not recommended as a treatment for which condition?
A. Osteoarthritis
B. Discospondylitis
C. Tendinopathy
D. Non union fracture
E. Pain relief
4. Which of the following is not an effect of ESWT treatment?
A. Stable cavitation
B. Inflammatory optimisation
C. Mechanotransduction
D. Photobiomodulation
E. Activation of growth factors and cytokines
5. When using ESWT you should:
A. Stop NSAID 48 hours before treatment
B. Hold the applicator at an angle of 45 degrees
C. Keep the applicator 3cm away from the skin and move continuously in a scanning pattern
D. Tell owners that symptoms will be relieved immediately
E. Start at a high frequency and gradually decrease after every 200 impulses
ANSWERS: 1C; 2B; 3B; 4D; 5A.