The Forgotten External Markers Of Clinical Disease
A clinical review by frontline clinician Dr Aine Seavers MVB MRCVS, for companion animal practitioners. Aine’s objective in this article is to bring the oft-forgotten nail examination back to centre stage, so that it remains a fixed component of any general health-check, carried out on any patient regardless of their health status on presentation
Part 1: The ‘not-so-humble’ Nail Clip
There is a mine of information in a nail clip. A nail examination is a wellness profile right in front of you, almost as good as any expensive blood screen.
If you firmly believe you would never fail your patients by compromising on pain prevention and pain management, then you have no choice but to always examine, and sometimes clip, your patient’s nails on most visits. Not checking the nails runs the risk you leave your patient still in pain, and most likely misdiagnosed and over-prescribed. Learn what is baseline-normal by doing nail clips on as many healthy animals as you can.
Once your nail examination fails ‘normal,’ suddenly you are potentially ahead of a simmering clinical condition to which the client is not yet alert. Equally, but especially in second opinion cases presented for gait or neurological abnormalities, a nail examination can reveal more than any advanced diagnostic imaging. Either of the above scenarios turn the now astonished client into a life-long customer of your practice.
External markers
There is a texture and a sheen to healthy nails and a healthy clicking ‘sound’ when you trim normal nails. Diseased nails lose all those healthy markers.
Sound: in Diabetes Mellitus and Hypothyroidism, you lose the ‘clicking’ noise. If you inspect these nails properly, you find that the nails are softer and that the quick is much narrower than normal. Question the client and without fail, the owner suddenly remembers to report that the pet is drinking more and urinating more.
Smell and touch: consider if the nail bed yeast infections you find are early indicators of allergy/atopy/contact-allergy/autoimmune disorders or canine hepatocutaneous syndrome; dependent on the age and breed of the pet.
Visual: dogs with skin allergy and infections often have various levels of gait disorder from co-existing pododermatitis. So, pay attention to gait and nails in any dermatology presentation and vice versa in an orthopaedic presentation.
Figure 1: Different variations of calving gates and crushes available.
Shredded nails can mean separation anxiety as well as recent trauma. Long over-grown nails means the animal is left alone for long periods of time or rarely if ever walked. This is an immediate alert to the vet that any treatment or protocols suggested to such an owner will most likely fail due to poor compliance by the owner.
That poor compliance may be disinterest on the owner’s part or may be an indicator that a genuine owner does not have control over the pet. If the latter, then a behaviour consultation becomes the priority before any other supportive protocols are attempted. Doing so makes for much better mental health for the dog, the owner and for the prescribing veterinary surgeon in the long run.
Long nails suggest the dog struggles to walk due to pain in their toes or because the overly long nails have physically bent the digits out of correct placement alignment.
I have lost count of the number of second opinions presented for recalcitrant lameness and/or episodic weakness or odd gaits, where supposedly nothing had been found on extensive physical and laboratory work-ups and now the clients were being referred for MRI. However, the MRI would also not have revealed a diagnosis – because the problem was not in the brain or spine etc – but rather with the paws and the nails, areas the previous vet had not bothered to check.
One recurring favourite find, in the second-opinion, episodic collapsing dog, is when you shave the long, usually matted fur and discover the cause of lameness: the over-long dewclaws interlocking on each other and binding the two legs together, causing the pet to collapse. Once the dog falls over, the hooked dewclaws slip apart and up the dog stands.
This ‘collapse’ can be recreated by the vet to demonstrate the issue to the client and then permanently resolved by simply clipping the offending nails. The consult air turns blue when the client realises that the treatment plan of the prohibitively expensive contrast myelogram/CT scan, should have instead commenced with a basic and affordable nail clip!
The examples above are a cautionary tale not to forget the dewclaws in any lameness issue.
A less dramatic presentation is a foreleg lameness from tendosynovitis in the abductor pollicis longus.
The forelimb dewclaws are not vestigial tissue, rather fully functioning ‘thumbs’ used extensively by most dogs from the pampered pooch holding its chew toy upright, a working rat dog terrier/Hund breed digging hard or a working patrol or farm dog or agility dog employing the stabilizer dewclaws in play and at work.
Failure to properly examine the dewclaws in either any front leg lameness or in a manic ‘licking of limb’ case presentation, means you may miss this primary trigger.
When manipulating the dewclaw and the carpus gently through a range of motion, ensure the dog is either muzzled or securing held. If the patient has ABL tendosynovitis, (De Quervain in humans), manipulating that tendon and/or carpus will induce a startlingly fast and damaging reaction from the dog.
Equally, old arthritic dogs who are not responding as expected to routine oral parenteral analgesic medications, PBMT/laser, supplements and diets, often just need to have their matted feet shaved back, enabling the dog to now stand and grip properly.
Clipping the overly long nails allows the animal to walk pain-free and with correct pad placement, none of which is possible in an animal with ‘wheelbarrow’ ingrown nails.
Parenteral medication has zero indication and zero efficacy in these nail conditions, whereas a proper nail clip and debridement provides immediate resolution of the pain and suffering.
So, next nail clip, engage your eyes, your ears and your sense of smell and touch.
Part 2: Nailing the Disorder
As our beloved UCD Professor JP O’Connor used to say: “Uncommon conditions occur more commonly than you think, if you actually took the time to look properly.”
Never is this truer than the condition known as Symmetrical Lupoid Onychodystrophy (SLO). Despite the complicated title and ugly acronym, SLO is a very clear-cut disease, of which the presenting clinical lesions would be seen by all of us in general practice in any given year, but more often than not, either dismissed by vets as irrelevant or unrelated in a lameness consultation. However, once you realise how SLO presents, you will never again miss or overlook this condition in a consultation.
SLO was first described by Professor Danny Scott in the early 1990s and describes a suspected immune-mediated condition that affects the claws, but spares the skin.
Rottweilers, German Shepherds, Labradors and Collies are over represented in a general small animal clinic setting. If being totally truthful, very few of us as general practitioners (non–Greyhound) would automatically put focal immune disease of the nail bed straight to the top of our differential for a lame dog. When we do see the odd broken nail, often with a shed nail beside it, we lean toward trauma or fungal/yeast conditions or nutritional issues, not to SLO.
SLO lameness starts in one foot and quickly spreads to the other feet, but not all nails get affected and not all to the same overt degree, as illustrated by some of the photos that follow. One clue is the ‘type’ of NSAID non-responsive pain and the associated lameness. This lameness is not the hot, hanging-limb lameness of an osteosarcoma, nor the head-dropping, dull throbbing lameness of most orthopaedic lesions. This pain is an exquisitely sensitive, almost stinging-like pain. The animal licks the affected nail constantly, is overly depressed and is lethargic, because whether moving or at rest, the lesions continue to be unrelentingly painful.
A visual clue is the classic ‘Popping the Hood/Bonnet” presentation. Once you see this on a non-dewclaw nail, you will never miss this presentation and clinical sign again.

Figure 13. ‘Popping the bonnet’ presentation, oncholysis.
It is wise to muzzle these dogs, regardless of their normal temperament and to first exam all the other nails, rather than the nails on the limb for which the client has presented the dog for lameness.
Check for missing nails, subtle cracks and fissures or splitting, then return to the most affected limb last. Usually, the cause of the intense licking and lameness is onycholysis and onychomadesis (shedding/casting of nail). The nails are hanging on proximally by shards of tissue, so every time the dog puts pressure on the limb; the half-shed nail sticks into the nail bed/corium which appears to be extremely painful.
While I have on occasion, removed a single severely onychomadetic nail by quick hand traction, it is preferable to deeply sedate or administer a light general anaesthesia to the pet before starting a proper work-up.

Figure 16. Traction-pulled nail.
To Biopsy or NOT to Biopsy?
Despite normally being an advocate for the usefulness of early biopsy in Derm cases, I canvassed the opinion of a large group of colleagues on this question as SLO is no routine biopsy procedure. The global experts just don’t bother with biopsy, in the words of one preeminent expert: “I think this diagnosis can be made on clinical grounds. The historical features and clinical appearance are pathognomonic in my experience. I would be surprised if any dermatologist can describe a case in which the characteristic clinical features were present, but an alternative diagnosis was made.”
With another specialist stating: “I always tell clients if my clinical dx is wrong and the dogs don't respond, we'll do the biopsy, but I haven't needed to follow up that way!”
In truth, SLO is like FAD. We could biopsy to confirm FAD in every FAD case, but such a classic inverted triangle of erythema and hypotrichosis in the caudal rump of a dog is so highly unlikely to be anything other than FAD, then no vet would consider a biopsy until such time as an effective flea allergy control regime first failed. Those same rules would appear to apply to the decision re: need or timing of biopsy for SLO.
The actual biopsy is either an amputated digit – usually a dewclaw is sacrificed – or else a modified cosmetic amputation to access an apyonchyia P3 for biopsy. In theory, a freshly-avulsed claw may carry viable claw bed epithelium/dermis and stand a chance at being diagnostic, but the success rate is 1/100.
Feedback from dermatohistopathologists is that a shed nail is useless as a biopsy sample, although examination of the shed nail could rule out dermatophytosis. Shed nails carry the risk of desiccation (and poor readability) of soft tissues, and secondary infections.
Protocol
1. Admit the patient to sedate and/or induce general anaesthesia.
2. Photographs. It is ideal to take photographs before any treatment is started since a photographic log is an excellent way to track the progress of this waxing and waning disease process.
3. If the dog had really been distressed by the unrelenting pain, then consider a local nerve block to give some additional pain relief during and on recovery.
4. Collect biochemistry including serum for T4/cTSH and consider the role of dietary intolerance/insufficiency in the clinical expression of SLO.
5. Skin scrapes, cytology, swabs for culture etc can then be taken carefully and safely.
6. Gently traction-pull the shedding or onychomachetic nails to remove the nail off the nail bed.
7. A sterile nail clippers and scissors can be used to separate the nail from any skin remnant.
8. Trim the remaining, less severely affected nails with a disposable grey 0.5 inch-wide emery board.
9. Shave the four feet to expose the ungula area of toe to gain better application of topical medications then and on-going at home applications.
10. Spray Cortavance on each affected nail bed and on the surrounding skin of toes.
11. Allow to dry fully, then just before the animal recovers fully from sedation, apply Aloveen lotion gently to affected areas.
Home application will be Cortavance daily for 21 days, then every second day on affected toes as needed. Feed or distract for 10 minutes after application to prevent the spray from being licked off.
For the dedicated owner and acquiescing dog, Aloveen lotion is applied gently to the sprayed areas some 30 minutes later. This is a bonus, not obligatory, as some patients will not tolerate their feet being handled much but especially so in the early days of recovery.

Figure 17. Shadows show onychoschizia or splitting.
Treatment
Treatments are many and varied and given this is a waxing and waning condition, often hard to accurately judge. I start off by adding Omega 3/6/EFA/Fish oil/Vit E to the diet. Virbac’s Megaderm Liquid is an excellent and simple first option. I upgrade the diet to Hills Z/D or Hills J/D.
I may use parenteral glucocorticoids early on in more severe presentations as much to get better compliance from the pet and the owner. However, my mainstay on these cases is the use of Cortavance Spray. The spray is licensed based on the absence of either thinning of the epidermis or suppression of the adrenal axis.
Cortavance is based on the prodrug HCA which has good penetration into the skin, then HC-17 propionate; the active drug has high anti-inflammatory activity in the epidermis, followed by acyl migration to a less active 21-propionate, which has zero local side effects in the dermis and then into a HC weak metabolite into the blood wherein it is conjugated and renally-excreted.
Concerns would be that:
1. The metabolism into a largely inactive metabolism in the dermis (which is why it’s safer), would mean that it could struggle to reach the deep germinal epidermis at the base of P3 in sufficient active concentration to be effective.
2. Applying a high concentration to the skin surface, could in theory, overwhelm the metabolic pathways, allowing deeper penetration, but this could negate the safety advantages.
However, Cortavance has been tested at up to 5x the dose without any demonstrated skin atrophogenicity at this concentration, suggestive of tolerance of this concentration.
Clinical systemic side effects would also be unlikely even at 5x the dose, as none were seen in Virbac’s safety studies, even when Cortavance was applied to one-third of the body surface area of the dogs.
In my cases, I am applying the medication to a much smaller surface area, reducing the likelihood there would be a significant adverse systemic effect
3. Many anti-inflammatory creams increase the risk of TEWL (transepidermal water loss), causing concern of additional nail cracking.
Virbac’s advice is that: “topical steroids like Cortavance can be used in conjunction with skin care where necessary (shampoos, moisturisers,) to avoid any concern over the skin drying effect of steroids and their excipients. The advantage of Cortavance over conventional steroids is that its fast absorption means that a moisturising lotion can be added 30-60 minutes later without the issue of diluting or interfering with the steroid.”
Over the years, I am having such a superb response to the Megaderm + Cortavance + Aloveen lotion combination, in uninfected SLO cases, that I have not had to progress to the other treatment options listed below.
Treatment options, all dispensed for a minimum of eight weeks, include:
The standard Tetracycline and Niacinamide (nicotinamide) every eight hours protocol. Concern re: antibiotic resistance means this option has fallen out of favour for many vets.
Some advocate for the use of Doxycycline in SLO, others only try it after Tetracyclines fail.
Azathiprine is occasionally used.
The Omega-3 fatty acid supplement is at an average dose of 180 mg EPA/7kg/day.
Biotin and gelatin may help. Avoid the feeding of raw egg as it binds biotin.
Pentoxifylline at 10-15 mg/kg tid may be of benefit.
It can take six months to see a maximum response to therapy so you just may need to be patient.
SLO can have an unpredictable heal-&-relapse pattern, with long periods of quiescence in between, which makes treatment additionally hard to assess. In some less severe cases, a few nails slough off, and these nails never grow back just leaving dried up quicks which at that level, don’t bother the dog. Many vets report that the nails never grow back properly and remain deformed.
My observation, using the Cortavance regime on nail beds that were first properly cleaned and debrided as above, is that the nails do grow back and do so with minimal deformities.
Finally, if the disease cannot be controlled medically and the dog is in intense continuous pain, remains lame, and constantly sheds nails, etc. then some vets will give consideration to surgically removing the nail beds. The latter is very much a last option salvage procedure pre-black bag and not one to be undertaken lightly, or early-on in the condition.

Figure 18. An example of a restrictive harness, correctly fitted, but still a problem for the dog.
Part 3: Nailing the Risk Factors – Restrictive Harnesses
I am developing major concerns about the increased popularity of restrictive leading harnesses –those that have a solid band horizontally across the front of the chest and anterior shoulder joint.
Yes, these harnesses do work as described, the dog can’t pull the owner along as easily on a walk, but at what cost to the proper skeletal development and function of the dog?
I truly believe no actively growing puppy dog should ever wear this restrictive style of harness ; due in no small part to its potential to place abnormal negative forces on growing bones and joints. If an owner has to use a restrictive harness on an adult dog, then seriously consider counselling them to either consider group training classes or private one-on-one dog training sessions, so as to train their dog to walk normally on a lead or Y-harness.
We began to see the appearance of odd deformities of the nails, pads and web skin disease, conditions that would relapse for no good reason, until we realised that these issues were the product of abnormal stance and abnormal contact. If you don’t make the connection – as we didn’t initially – the dogs may go on to present with an unusual run of broken/avulsed toenails, first on one foot, then another foot. These nails are trauma shattered or avulsed in a manner very different to an SLO presentation.
Perhaps, these broken nails are a manifestation of the collateral damage from altered forces, wherein the main weight bearing legs (i.e., forelimbs) that take 66 per cent of the weight-bearing load in a non-obese pet—can’t themselves get the full range of movement through the shoulder joints, so the back legs start to incur abnormal forces as well.
There is no ‘popping the bonnet ’ appearance of the nail as in SLO. The nail itself is not diseased as in SLO.
The restrictive harness allows owners to walk their dogs farther as it is now easier on the owner, but harder on the poor hobbled creature walking beside them. This means these dogs are walked for longer and on different terrains, resulting in a perfect storm for lesions to occur due to increased contact and increased exposure to different surfaces.
Next time you see or indeed fit a dog with one of these restrictive body harnesses, watch the dog from side-on to see how they move in this device.
You don’t have to be a vet to realise the dog is being effectively hobbled:
The dogs are unable to fully extend their shoulders and elbows out into a normal stride gait.
Additionally, the dog’s neck is held higher and the head more rigid than when fitted on a Y-shaped old-style harness.
The pet’s neck appears to bob up and down more around the C6-C7 articulation.
C6-C7 is not a good anatomical place on which to place abnormal wear and tear in general, but especially not in puppies and in larger breed dogs.
Often the tail is held down tight into the body, perhaps in order to counterbalance the higher and extended head position at the other end.
The toes are often over-extended and end up splayed-out to provide balance. As a result, the side toes, usually the non-major weight bearing toes are now weight-bearing. Given that canine skin is one-twentieth of the thickness of human skin, even the slightest sustained off-balance wear can trigger an issue from a friction pressure that might not even be detected on a pressure-plate reading.
To see why you should not use a harness, that goes across the chest of a dog, see the video at this link: https://www.facebook.com/HydrotherapyForDogs/videos/278711409626940
Prevention via Y-shaped harnesses
Initially, in some dogs, these Y-harnesses may temporarily restrict the range of joint movement, often simply because the dog has to get used to the odd feel of walking on any harness. However, should the dog really need to fully extend its front limbs for whatever reason, it can do so on a correctly-fitted Y-harness,.
The head, neck, toe and tail gait on a Y- harness more closely resemble that of a normal walking gait. The Y-harness must have the front band neat and snug against the sternum and neck. It must not hang down loose over the shoulders otherwise this loose, low-slung position will act as a de facto restrictive harness.
It is better to have an open-and-clip adjustable close set-up on the harness, rather than a fixed frame that fits over the head. I find these larger, fixed-frame harnesses often sit too low down on the shoulders and are often over-heavy, especially for the smaller breeds. We prefer the softer, light seat-belt material type of Y-harness rather than these heavier solid, almost saddle-like versions, that dogs often present wearing.

Figure 19. Tyson is wearing a correctly fitting Y shaped harness. The point of the lead attachment is at the centre of gravity-which sits mid shoulder so the pull is from there, from the strongest part of the body-not encircling the neck nor trapping the shoulder, nor focused on the anticlinal vertebrae–the latter area I would not like to have pressure on in any dog, regardless of its I.V.D.D risk.
Part 4: Fixing the Floor Issue
The move to carpet-free flooring in houses can be great for a dog with allergies but woeful for a pet’s normal stability and gait. The shiny slippery surfaces cause anything from minor or major disruption to households and compromised pet welfare in terms of limiting ‘the where, the when and the degree’ to which pets can chose to interact with their owners.
Some animals will simply choose to withdraw into safer zones, resulting in less spontaneous pet-human social interaction and with greater stress and anxiety for the pet. Some pets will struggle on and many clients of elderly dogs often seem either oblivious or else overwhelmed to how difficult it is for their dogs to safely and securely transition around the house.
Often elderly pets will present as developing a poor appetite, when in fact theys have a great appetite, but just don’t have the strength to hold themselves upright for extended periods on a slippery floor to access their floor-based food bowls. Elevate the food bowls, plus place non-slip mats in a generous arc around the bowls and the ‘inappetence’ disappears before your eyes.
Younger dogs often seem to become airborne on the wooden/tile floors, then slide and/or slam into a door or furniture resulting in injury.
There are several work-arounds to making the floors safe and less slippery for the family pets. I have included my clients’ four most popular options below.
Solution 1: Cheap and Easy Anti-Slip Strips
A trip to the shops to purchase as many metres of anti-slip underlay as needed by the owner in the colour of their choice will resolve many issues. Owners then can create a cheap washable replaceable walkway against any wall or create transition walkways and paths to other areas to allow the pet to traverse across the slippery floors.
While the same grip principle applies to non-slip dog socks and boots for pets, my clients find the socks grip, but the dog just rotates around in the sock and then the sock falls off. The home-made anti-slip mat runways, custom-cut to the width and length needed for each house and for each pet, work much better.
Solution 2: Carpet Runners
For larger or heavier dogs, you may need to also use a carpet runner, on top of the anti-slip underlay for better traction.
Household supply stores sell a variety of 60cm-wide (approximately) rolls of carpet runner in various colours and designs you can have cut to the required length to then sit on the underlay so the carpet runner does not slide.
Solution 3: Paw Pads
PawFriction is a paw pad coating designed for senior dogs to help with traction on slippery surfaces.My initial reaction to this product was negative, amid concerns it could cause reactions on the pads or if it was ingested.
I asked around and got the following feedback from a vet colleague: “It seems to help my elderly dogs walk on my vinyl floor with less slipping. They didn’t lick at it or seem bothered and it was easy to apply, though a bit messy. Downside is, it only lasts about a week and has to be reapplied.”
Given the distress and exhaustion otherwise healthy old dogs experience trying to get weak legs under them, the product is still worth considering.
Solution 4: Dog boots/shoes
While there are many dog boots/shoes around now, many are not so good indoors.
One option work considering are disposable rubber slip-on boots that claim to give traction on slippery surfaces, for details see www.pawzdogboots.com.
Don’t leave the product on the dog unsupervised as it could represent an intestinal blockage risk if eaten and obviously don’t leave it on for too long so that the dog runs the risk of developing circumferential pressure sores.
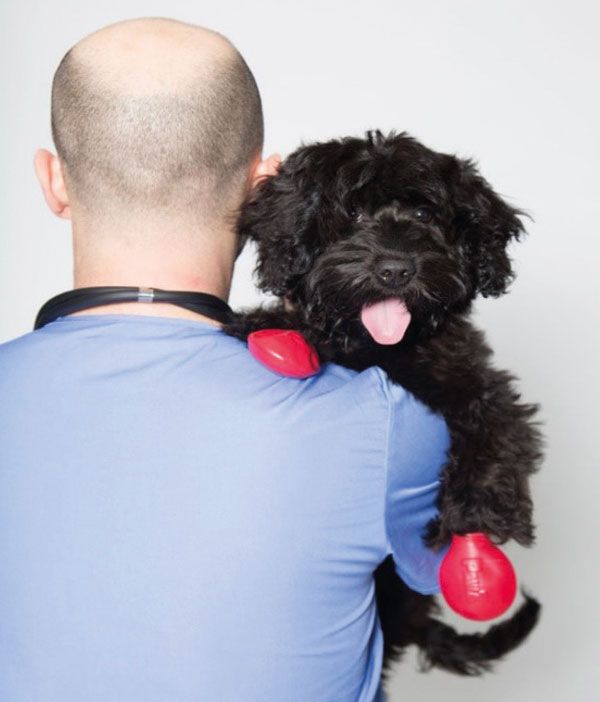
Figure 25.
Acknowledgements
My thanks to Dr Guillermino Manigot for Figures 1 to 8 and to Dr K Coyner, Dr R McFadden, Dr T Bord and Dr R Hilton for the cat nail images. Thank you to Dr Emily Rothstein Bassell for details of the website for disposable rubber slip-on boots.
1. Name a focal immune disorder of the nail bed:
A. Shredded nails
b. Long overgrown nails
C. Symmetrical Lupoid Oncychodystrophy (SLO)
D. Discoid Lupoid Erythematosus (DLE)
2. Which three of these dog breeds are at higher risk of SLO?
A. Bichon Frise
b. Rottweiler
C. German Shepherd
D. Labrador Retriever
E. Cavalier King Charles Spaniel
3. Name two diseases that can target the feline nail bed:
A. Feline Lymphoma
b. Feline Pemphigus foliaceus (PF)
C. Feline Proliferative Necrotising Otitis
D. Feline Lungworm Disease
4. Which of these two possible concerns are raised by the finding of shredded nails in a canine patient?
A. Malassezia infection
b. Recent trauma
C. Prolonged inactivity
D. Separation anxiety
5. Name two clinical observations that should be a mandatory part of any gait or neurological veterinary examination?
A. Culture of nail clippings
b. Assessment of the appearance of all nails, including the dewclaws
C. Listening to the sound of the nails hitting the ground as the dog walks
D. Assessment of the style of walking restraint used on the pet
6. How can a diagnosis of SLO usually be made?
A. Only by biopsy of a single nail
b. Only by biopsy of an entire amputated P3 along with nail
C. On clinical grounds without biopsy
D. Fine needle aspirate of nail bed
Answers: 1C; 2B, C and D; 3A and B; 4B and D; 5B and D; 6C.


































