The jaundiced cat – differentials and clinical approach
Monica Augusto DVM MSc Dip-ECVIM PGDipUTL MRCVS, lecturer in small animal internal medicine at University College Dublin, presents a brief review of the medical approach to cats with jaundice
Jaundice, or icterus, refers to the yellow discoloration of the mucous membranes, sclera, and skin, and it represents a clinical manifestation of hyperbilirubinaemia9. By being aware of the metabolism of bilirubin, it is possible to approach cats with jaundice in a systematic order, and divide the cases in pre-hepatic, hepatic and post-hepatic jaundice. This review article summarises the main differentials for feline hyperbilirubinaemia and its clinical approach.
Bilirubin metabolism
Most bilirubin results from red blood cells (RBC) degradation, either through normal quiescence (removal of aged RBC) or abnormal RBC destruction (haemolysis). The first step occurs within normal macrophages, where the free heme group of the RBC is oxidised to biliverdin. The iron is released and potentially stored. The biliverdin is reduced to unconjugated bilirubin, and subsequently released into plasma, where it binds to albumin, and is carried to the liver. To become conjugated bilirubin, the hepatocyte removes the bilirubin from the albumin and processes the bilirubin for excretion into the biliary system (which is the rate-limiting step of the entire bilirubin metabolism pathway). Bilirubin is excreted, along with bile salts, into the intestine where bacterial and intestinal enzymes reduce conjugated bilirubin to urobilinogen. Urobilinogen is reabsorbed (about 10 per cent) or broken down (90 per cent) into urobilin and stercobilin (both of which are excreted in the faeces). Of the resorbed urobilinogen, most is taken up by the liver again (enterohepatic circulation), while the rest bypasses the liver and is excreted into the urine 1.
Differentials for hyperbilirubinaemia in cats
There are three pathophysiological mechanisms of hyperbilirubinaemia and jaundice. Pre-hepatic, hepatic and post-hepatic jaundice causes are described in Table 1.
When bilirubin concentration exceeds the 35μmol/L jaundice becomes visible 9,10. However, jaundice is not a sensitive or specific marker of disease; for instance, cats can have severe liver disease and not be jaundiced, and similarly, the differentials for any type of jaundice is not limited to one specific condition. Moreover, it is frequent for cats to present with multiple concurrent underlying problems.
Because the normal feline liver has a high capacity to process large amounts of bilirubin, jaundice only occurs when there is overwhelming haemolysis, significant decrease in hepatic function and/or obstruction to normal bile flow. It is also worth mentioning that a fraction of conjugated bilirubin can bind irreversibly to albumin (as delta-bilirubin). If that happens, that fraction of bilirubin may remain in circulation for the same length of time as albumin (approximately two-weeks)7, so the jaundice might be visible on physical examination even after resolution of the underlying disease.

Figure 1. Jaundiced skin of a cat with extra-hepatic bile duct obstruction due to acute necrotising pancreatitis, and concurrent hepatic lipidosis. Picture courtesy of Dr Ana Jacinto MRCVS.
Cholestasis of sepsis in cats
Note that a septic cat may have hyperbilirubinaemia (although often no visible jaundice) without having a structural hepatobiliary disease or haemolysis2. For example, cats presented with pyothorax, abscesses or significant tissue necrosis. That can happen because of complex changes in bilirubin metabolism within the hepatocytes due to cytokines and endotoxins, nutritional changes, and cats intrinsic low concentration of glucuronosyltransferase (liver enzyme needed to conjugate bilirubin).
Diagnostic approach
The diagnostic approach should take in to consideration the signalment, clinical history and physical examination findings. Diagnostic tests and procedures aim at:
firstly, recognising cases with pre-hepatic jaundice;
differentiating between hepatic and post-hepatic jaundice; and,
ultimately identifying the underlying cause, keeping in mind that more than one type of jaundice can be present concomitantly.
Signalment
It is important to consider the age and breed of the animal when assessing for any clinical sign, including jaundice. For instance, Bengal, Abyssinian and Somali cats have a predisposition to erythrocyte pyruvate kinase (PK) deficiency3, which is an inherited erythrocyte disorder, and are usually presented with anaemia at a young age. Older cats are more likely to have a neoplastic disease. Abyssinian and Somali cats are also seen more often with erythrocyte osmotic fragility syndrome 12, another cause of pre-hepatic haemolysis and jaundice. Siamese cats are predisposed to hepatic amyloidosis, a known cause of hepatic jaundice.
Clinical history
A comprehensive clinical history is an essential step in the diagnostic process of any animal and allows the formulation of a thorough investigation plan. Clinical signs in jaundiced cats might be vague, such as lethargy and anorexia (even though those might be the only signs of anaemia in cats), or be directly associated with the underlying cause, for example vomiting and diarrhoea in cats with inflammatory liver disease. Also, non-specific signs of intoxication and acute liver failure (e.g., vomiting, dull mentation) might be observed in cats that have ingested certain drugs and/or toxins.
During the clinical history, it is important to remember that the owner’s ability to provide accurate information about frequency, chronicity, and severity of the clinical signs may be affected by the cat’s outdoor access and multi-cat households. The following topics should be covered during a good clinical history:
indoors vs outdoor access;
lethargy;
hyporexia or anorexia;
weight loss;
presence of vomiting and/or diarrhoea;
current treatments;
post prandial behaviour and/or neurological signs;
exposure to potential hepatotoxic drugs, supplements, or nutraceuticals;
exposure to environmental toxins;
other non-gastrointestinal clinical signs.
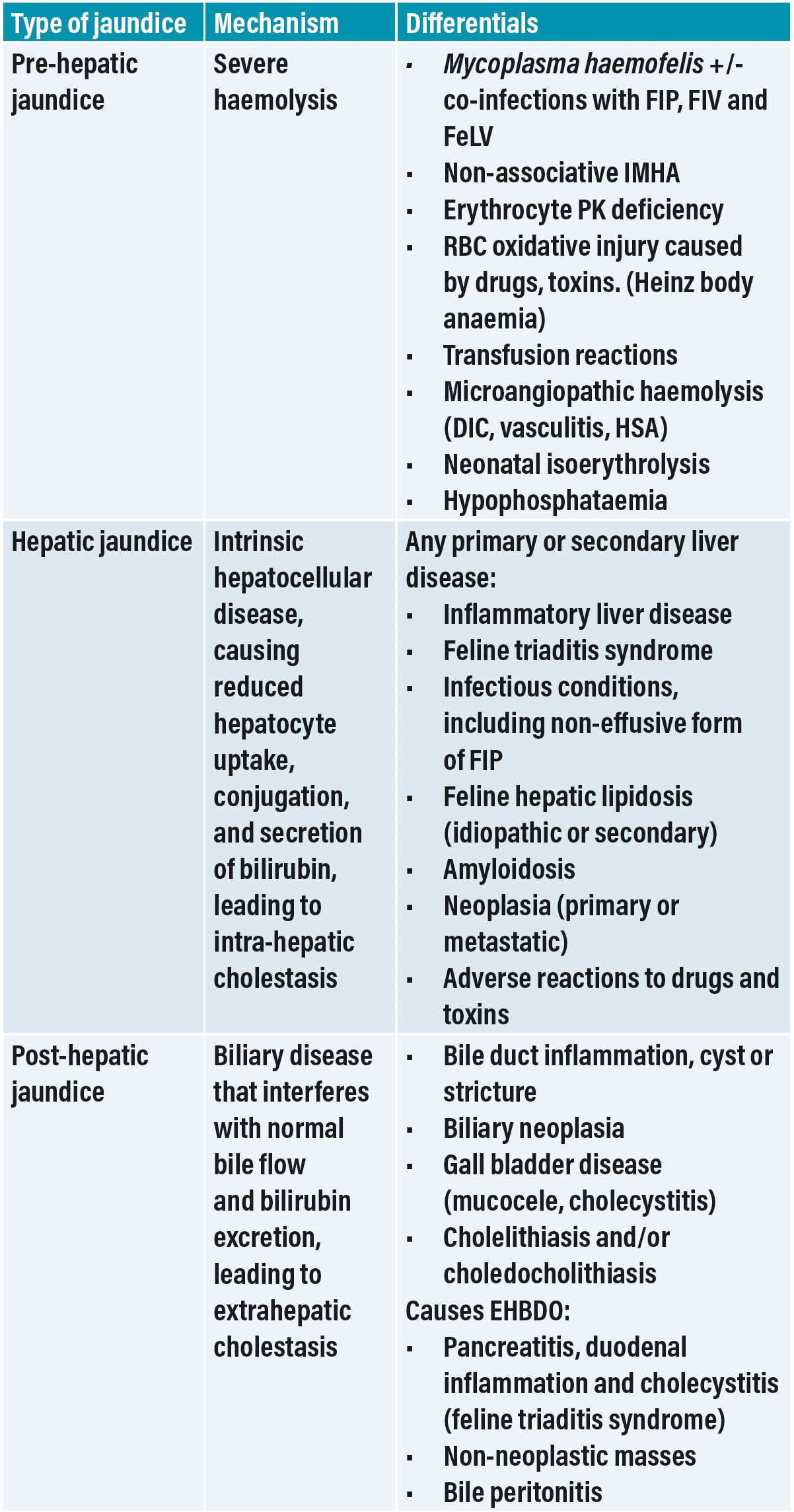
Table 1: Main differentials for pre-hepatic, hepatic and post-hepatic jaundice in cats, and the pathophysiologic mechanisms leading to the development of hyperbilirubinemia and subsequent jaundice. Feline triaditis is the concurrent manifestation of inflammatory bowel disease, cholangitis and pancreatitis, and can lead to post-hepatic jaundice.
DIC = disseminated intravascular coagulation; EHBDO = extrahepatic bile duct obstruction; FIP = feline infectious peritonitis; HAS= haemangiosarcoma; IMHA = immune-mediated haemolytic anaemia; PK = pyruvate kinase.
Physical examination findings
A complete physical examination, including cardiovascular assessment, abdominal palpation, and body temperature, as well as fundic examination should be carried out in all cats with jaundice. Jaundiced cats with severe anaemia (i.e., pre-hepatic jaundice) are likely to be tachycardiac and may have a cardiac murmur. Cats with EHBDO due to acute pancreatitis may show abdominal discomfort/pain on palpation, while cats with hepatic lipidosis, inflammatory liver conditions or diffuse neoplasia (e.g., lymphoma) may have hepatomegaly.
When primary hepatobiliary disease is suspected, cats may exhibit:
jaundice;
hepatomegaly on abdominal palpation;
abdominal discomfort or pain;
poor overall condition, coat or body condition score (BCS);
fluid thrill (if ascitic);
pyrexia.
Cats with sepsis (for example, secondary to acute neutrophilic cholangitis) may exhibit bradycardia, hypotension, or be presented collapsed.
Diagnostic tests and procedures
The first step in the diagnostic investigations should be to exclude a severe anaemia (i.e., pre-hepatic jaundice). Significant RBC destruction is usually associated with a decrease in haematocrit or packed cell volume (PCV). In the absence of anaemia, the second step should be an abdominal ultrasound to distinguish between hepatic and post-hepatic jaundice, although imaging would also be required to investigate for an underlying cause of haemolysis.
a. Clinicopathological evaluation
A complete haematology and biochemistry profile helps to classify the types of jaundice, and often excludes a pre-hepatic cause. However, the interpretation of the haematology results should take into account the clinical history (e.g., chronicity of signs, clinical progression) and physical examination findings.
Blood smear examination helps to characterise the type of anaemia, as well as to identify haemoparasites. The anaemia in cases of pre-hepatic jaundice is normally regenerative as it is due to overwhelming haemolysis. Additional diagnostic tests are then required to find an underlying cause or trigger (e.g., Coombs’ test, thoracic and abdominal imaging, urine culture, etc). A positive polymerase chain reaction (PCR) test for Mycoplasma haemofelis confirms the diagnosis in most cats with haemoplasma infection.
Upon evaluation of serum biochemistry, it is important to remember that even small increases in liver enzyme activities are clinically significant in cats because the half-lives of most feline enzymes are very short compared to dogs (e.g. t1/2 of ALT and ALKP are approximately six hours in cats vs. 2.5 days and 70 hours, respectively in dogs)2. In addition, the assessment of liver function in jaundiced animals should not be done by means of bile acid stimulation test, but instead be determined by the evaluation of all other biochemical parameters (such as, albumin, urea, cholesterol, glucose, ammonia concentration).
Haemostasis can be affected by cholestasis and hepatic function, so basic coagulation profile – activated partial thromboplastin time (aPPT) and prothrombin time (PT) is routinely recommended.
Lastly, it should be noted that cats have a high renal threshold for bilirubin excretion and any amount of bilirubin detected in the urine is always abnormal 10.
b. Abdominal imaging
A careful examination of the entire biliary system can be performed during abdominal ultrasonography with the aim of excluding an obstructive disease. Focal liver lesions and other potential causes of EHBDO can also be identified. However, cats frequently have concurrent hepatic and post-hepatic conditions, and recognising the instigating cause can be challenging (e.g., cats with triaditis or EHBDO may develop concurrent hepatic lipidosis).
c. Sampling (fine-needle aspirates, biopsies and cholecystocentesis)
The overall agreement between histopathology and cytology interpretation of ultrasound-guided, fine-needle aspirates (FNAs) of the liver in cats was found to be only 51.2 per cent, with the best agreement seen in cases with hepatic lipidosis and neoplasia14. However, FNAs are less invasive and generally don’t require a general anaesthetic.
Hepatic biopsies are often crucial to obtain a definitive diagnosis of intrinsic liver disease (i.e., underlying cause of hepatic jaundice). Indications and guidelines for hepatic biopsies have been published by the WSAVA liver standardisation group in 2006 8. Feline histopathological samples can be obtained by percutaneous Tru-cut ultrasound-guided biopsies (using 16 G needle for cats), or surgical techniques. There are certainly advantages and limitations for each biopsy method, but even percutaneous ultrasound-guided liver biopsies in cats have a low risk of bleeding and development of severe complications 6. Regardless of the technique, it is important to maximise the value of the procedure to obtain good and adequate size biopsies, ideally from multiple liver lobes 5.
For cats with suspected bacterial cholangitis/cholangiohepatitis, cholecystocentesis is more likely to yield a positive bacterial culture than liver tissue culture13. Furthermore, percutaneous ultrasound-guided cholecystocentesis was reported to have a low complication rate (3.4 per cent) 11 and should be considered in most cats that undergo liver biopsies.
A combination of tests is usually necessary during the clinical investigations of cats with jaundice (Table 2).
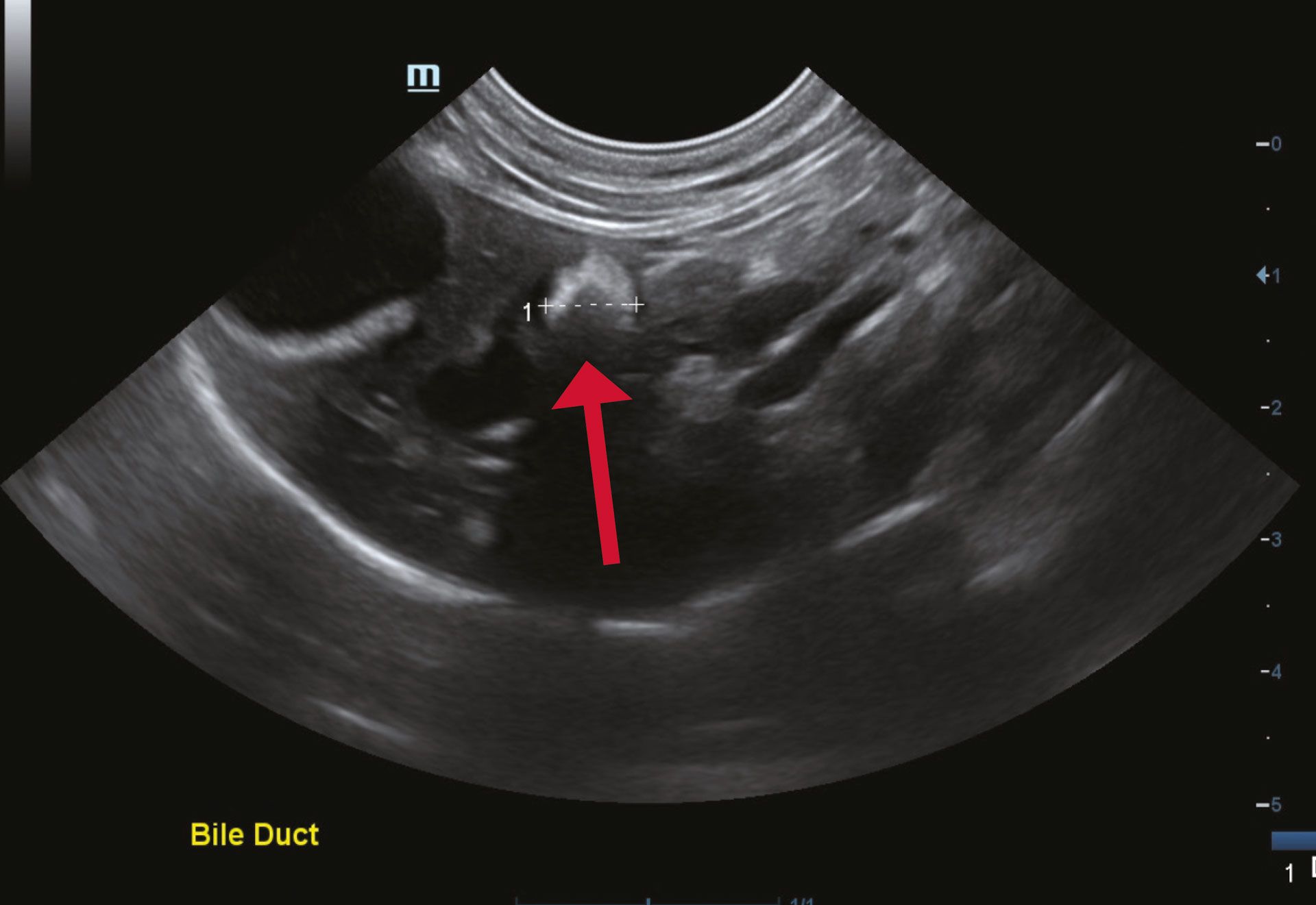
Figure 2. Cat presented with marked jaundice and vomiting. Abdominal ultrasonography showed significant intra-hepatic bile duct dilation due to a large cholelith (red arrow); Image courtesy of Dr Ana Jacinto MRCVS.
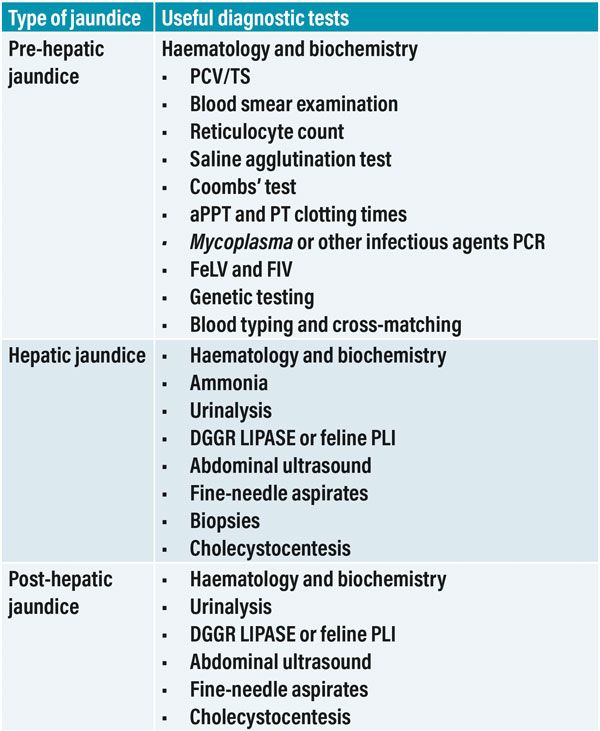
Table 2: List of routine diagnostic tests often performed during the clinical investigation of cats with jaundice.
aPPT = activated partial thromboplastin time; FeLV = feline leukaemia virus; FIV= feline immunodeficiency virus; PCV/TS = packed cell volume/total solids; PT = prothrombin time; PCR = polymerase chain reaction.
-
Bilirubin. Eclin Path Cornell University College of Veterinary Medicine. Available from: https://eclinpath.com/chemistry/liver/cholestasis/bilirubin/
-
Cocker S and Richter K. In Textbook of Veterinary Internal Medicine. 8th ed. St. Louis: Saunders Elsevier, 2017. Section XIX, Chapter 280. Hepatobiliary disease. Diagnostic Evaluation of the liver; pp 1611-1621.
-
Grahn RA, Grahn JC, Penedo MC, Helps CR and Lyons LA (2012) Erythrocyte pyruvate kinase deficiency mutation identified in multiple breeds of domestic cats. BMC Veterinary Research 8:207-217. doi.org/10.1186/1746-6148-8-207
-
Koster L, Shell L, Illanes O, Lathroum C, Neuville K and Ketzis J (2016) Percutaneous ultrasound-guided cholecystocentesis and bile analysis for detection of Platynosomum spp.-induced cholangitis in cats. Journal of Veterinary Internal Medicine. 30(3):787-793 . doi: 10.1111/jvim.13943
-
Lidbury A . (2017) Getting the most out of liber biopsy. Vet Clin North Am Small Animal Practice 47(3):569-583 doi: 10.1016/j.cvsm.2016.11.007Pavlick M, Webster C,
-
Penninck DG (2019) Bleeding risk and complications associated with percutaneous ultrasound-guided liver biopsies in cats. Journal Feline Medical Surgery. 21(6):529-536. doi: 10.1177/1098612X18788883
-
Rothuizen J (2009) Important Clinical Syndromes associated with liver disease. Vet Clin North Am Small Animal Practice 39: 419-437. doi: 10.1016/j.cvsm.2009.02.007
-
Rothuizen J, Desmet VJ, van den Ingh T, Twedt DC, Bunch SE and Washabau RJ. Sampling and handling of liver tissue. In: WSAVA standards for Clinical and Histological diagnosis of canine and feline liver diseases. St. Louis: Elsevier, 2006, pp 5-14.
-
Sherding RG (2000) Feline jaundice. Journal Feline Medical Surgery 2(3):165- 169. doi.org/10.1053/jfms.2000.0088
-
Sherding RG. Icterus. In Washabau RJ and Day MJ (eds): Canine and Feline Gastroenterology. St. Louis: Elsevier, 2013, pp 140-147.
-
Smith RP, Gookin JL, Smolski W, Di Cicco MF, Correa M and Seiler GS (2017) Association between Gallbladder Ultrasound Findings and Bacterial Culture of Bile in 70 Cats and 202 Dogs. Journal of Veterinary Internal Medicine 31(5): 1451–1458. doi: 10.1111/jvim.14792
-
Tritschler C, Mizukami K, Raj K, Giger U (2016) Increased erythrocyte osmotic fragility in anaemic domestic shorthair and purebred cats . Journal Feline Medical Surgery 18(6):462-470. doi: 10.1177/1098612X15587574
-
Wagner KA, Hartmann FA and Trepanier LA (2007) Bacterial culture results from liver, gallbladder, or bile in 248 dogs and cats evaluated for hepatobiliary disease: 1998-2003. Journal of Veterinary Internal Medicine. 21(3):417-24. doi: 10.1892/0891-6640(2007)21[417: bcrflg]2.0.co;2
-
Wang KY, Panciera DL, Al-Rukibat RK and Radi ZA (2004) Accuracy of ultrasound-guided fine-needle aspiration of the liver and cytologic findings in dogs and cats: 97 cases (1990–2000) Journal of American Veterinary Medical Association 224 (1): 75-78 doi.org/10.2460/javma.2004.224.75
-
Webb CB (2016) The yellow cat: diagnostic and therapeutic strategies. Today’s veterinary practice 38-50.
1. A cat is presented with a chronic history of intermittent pyrexia and mild jaundice, and you are explaining your diagnostic plan to the owner. Which of the following statements is CORRECT?
A. Jaundice is highly specific biomarker for intrinsic liver disease
b. Jaundice is highly specific biomarker for immune-mediated haemolysis
C. Jaundice is a highly sensitive biomarker for hepatobiliary disease
D. Jaundice is a poorly sensitive biomarker for hepatobiliary disease
2. Which of the following initial diagnostic tests is the most cost effective in a cat with expected pre-hepatic jaundice?
A. Haematology and Coombs’ test
b. Packed cell volume (PCV) and blood smear examination
C. Serum biochemistry profile and blood smear examination
D. Coombs’ test and abdominal imaging
3. Which of the following infectious agents is considered a common cause of haemolytic anaemia in cats?
A. Feline leukaemia virus
b. Mycoplasma haemofelis
C. Feline infectious peritonitis
D. Aelurostrongylus abstrusus
4. A young cat is presented with acute onset of vomiting and jaundice. Following initial diagnostic investigations (including bloods and abdominal ultrasound) you suspect the cat might have inflammatory liver disease. What would be the most appropriate less invasive diagnostic plan for this cat?
A. Percutaneous ultrasound-guided fine-needle aspirates and cholecystocentesis
b. Liver wedge surgical biopsy for histopathology and tissue culture
C. Start empirical treatment with antibiotics and steroids
D. Test for pancreatitis and cobalamin measurement to exclude feline triaditis
5. What result would preclude a diagnosis of post-hepatic jaundice?
A. Normal abdominal radiography
b. Normal abdominal ultrasonography
C. Absence of cholelithiasis on abdominal ultrasound
D. Absence of tumour on abdominal ultrasound
Answers: 1D; 2B; 3B; 4A; 5B.














