Diagnosis and treatment of feline hyperthyroidism
Vanessa Bourne MVB CertAVP(SAM-F) PGCertVetEd FHEA MRCVS, discusses the diagnosis and management of feline hyperthyroidism
Hyperthyroidism is not an uncommon disorder of older cats in Ireland but is anecdotally considered of low prevalence. In one study, a high proportion of hyperthyroid cats (in excess of 60 per cent) did not have a palpable goitre. Given that around 90 per cent of hyperthyroid cats in other studies have palpable goitre, this discrepancy may reflect the considered low prevalence of disease. If goitre is not palpated, clinicians may not include hyperthyroidism in their list of differentials and not consider testing total thyroxine. Clinicians are advised to spend sufficient time during routine and non-routine checks palpating the thyroid area. It is good practice to consider measuring total thyroxine in cats aged seven and older.
Untreated cats with hyperthyroidism will suffer considerable morbidity from their disease, both reversible and irreversible. Therefore, it makes good sense from a patient welfare perspective to identify these cats earlier and implement treatment regimes. It is also good business sense to identify and treat these patients as they represent a good income stream to the practice. Cat-only clinics and cat geriatric clinics are worth considering as they can increase revenue and can be readily implemented. Creating a cat-only area reduces stress and anxiety in the patient and owner, and allows for improved examinations and more accurate results from sampling.
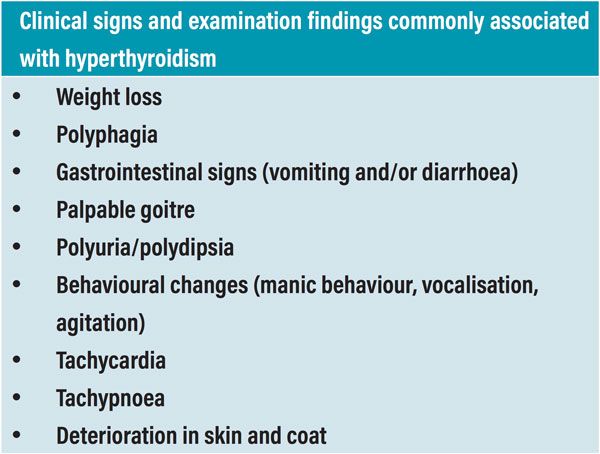
Table 1.
What is hyperthyroidism?
Hyperthyroidism is an endocrine disorder of older cats, resulting from excess circulating thyroid hormone concentrations (triiodothyronine [T3] and/or thyroxine [T4]) produced by abnormal thyroid tissue. Most cats with hyperthyroidism have benign adenomatous hyperplasia with <2 per cent having thyroid carcinoma.
Thyroxine (T4) is the major hormone secreted by follicular cells of the thyroid gland, however the metabolite triiodothyronine (T3) is responsible for most of the hormonal activity. Once thyroid hormone has entered the target cell, it may exert its biologic effects controlled by enzymes. Secretion of thyroid hormones is under the control of TSH (thyroid stimulating hormone) secreted by the anterior pituitary gland, which is in turn controlled by TRH (thyrotropin releasing hormone) secreted by the hypothalamus. These hormones operate on a feedback system. Measuring TRH in practice is difficult but TSH can be measured easily. There is not currently a feline-specific TSH assay available and assays used for measuring canine TSH are currently utilised. In cases of hyperthyroidism, TSH should be suppressed. TSH is most often used to help determine whether a patient is clinically hypothyroid (TSH will be increased and T4 will be below normal range) following a permanent treatment for hyperthyroidism.
Clinical signs and examination findings commonly associated with hyperthyroidism:
Hyperthyroidism is traditionally a disease of older cats. The classic presenting signs of feline hyperthyroidism are listed in Table 1.
In patients with the uncommon, apathetic form of hyperthyroidism, lethargy and inappetence are present, instead of the more classic presentation findings.
Comorbidities and differential diagnoses to consider with hyperthyroidism
Differential diagnoses to consider for cats presenting with similar signs of hyperthyroidism include diabetes mellitus, chronic kidney disease (CKD), chronic enteropathies, lymphoma and parasitism. Therefore, a thorough examination of the patient is required to identify any comorbidities rather than adopting a pattern recognition approach and potentially missing concurrent disease.
Hypertension may be present together with hyperthyroidism (estimated at 10 to 13 per cent). Blood pressure should be measured routinely in mature patients, together with fundic examination to examine for potential signs of target organ damage.
In many cases, hypertension diagnosed with hyperthyroidism will resolve with treatment of the hyperthyroidism. Where it does not, assessment of the patient for concurrent diseases that commonly cause hypertension should be made (CKD being the most common, primary hyperaldosteronism, hyperadrenocorticism or phaeochromocytoma).
Where the patient is markedly hypertensive or there is evidence of target organ damage, antihypertensive treatment would also need to be instigated while treating the hyperthyroidism. Interestingly, some patients may develop hypertension once euthyroidism has been achieved (up to 25 per cent). Therefore, it is recommended to measure blood pressure approximately six weeks into treatment, even if blood pressure was normal previously.
Palpation of a swelling in the neck area may be an enlarged thyroid gland but can also be due to physician error (feeling normal anatomy), abscessation, cyst or neoplasia. Thyroid glands may be enlarged but not secreting excessive thyroid hormones also.
Thyroid hormone has a positive chronotropic effect and the disease has multiple effects on the cardiovascular system. These include: increased beta-adrenergic activity and activation of the renin-angiotensin-aldosterone system, alongside a decrease in systemic vascular resistance, and increasing cardiac output and heart rate. Therefore, a tachycardia is one of the most frequently reported physical examination findings. Hyperthyroidism can also cause left ventricular hypertrophy. Cardiac murmurs and arrhythmias (typically a gallop rhythm) may also be auscultated. Echocardiography and electrocardiography can provide additional information in these cases. The degree of cardiac remodelling is dependent on patient factors and the extent of thyroid disease progression. Some changes may be reversible if the disease is caught early and successfully managed.
Glomerular filtration rate (GFR) is increased in cats with hyperthyroidism while muscle mass is typically reduced. Therefore, it is possible that creatinine measurements will increase following treatment of hyperthyroidism. This should be interpreted as a true reflection of the patient’s renal function and not a deterioration associated with treatment. Patients should receive treatment for hyperthyroidism even if they have impaired renal function, as the hyperthyroid state is likely to cause ongoing glomerular hypertension and hyperfiltration, leading to progression of renal disease.

Table 2.
Diagnosis of hyperthyroidism
Diagnosis of hyperthyroidism is made based on a persistently elevated total thyroxine (TT4/T4) measurement or a high normal TT4 in combination with an elevated free T4, in combination with one or more clinical sign. Previously, we tended to measure TT4 in cats only when hyperthyroidism was suspected or when patients were quite mature as part of a normal screening. However, now it is more commonly recommended to monitor TT4 from the age of seven. An increasing TT4 measurement over time can heighten the suspicion of the early development of hyperthyroidism. Thyroxine measurement at a reference laboratory is highly recommended rather than using in-house analysers for accuracy.
An ideal minimum database should consist of haematology and biochemistry samples, alongside T4, blood pressure measurement and urinalysis.
Erythrocytosis and macrocytosis have been found in cases of hyperthyroidism. If a patient presents with anaemia, they should be evaluated for concurrent disease. Elevations in liver enzymes are very common; if these do not resolve with successful treatment of hyperthyroidism, further evaluation of liver parameters and function is warranted. Urine specific gravity may be <1.030 due to effects of hyperthyroidism causing polydipsia. Patients’ renal function should always be examined as part of initial assessment and as part of monitoring of treatment.
The 2016 AAFP (American Association of Feline Practitioners) Guidelines for the Management of Feline Hyperthyroidism (hereafter referred to as the Guidelines) formulated a simplified approach to diagnosing hyperthyroidism, categorising patients into one of six categories, as discussed overleaf.
Group 1: Cats with classic clinical disease
These patients will have clinical signs commonly associated with hyperthyroidism and a persistently elevated TT4. Cats should be treated for their hyperthyroidism and any concurrent disease considered.

Table 3.
Group 2: Cats with possible hyperthyroidism with other non-thyroidal illness
Cats in this category have a TT4 within the reference interval and clinical signs suggestive of hyperthyroidism.
In this situation, the following approaches are recommended:
Re-measurement of TT4 alongside free T4 by equilibrium dialysis (fT4ed) two to four weeks after initial testing. A TT4 value in the upper half of the reference range together with an elevated fT4ed supports a diagnosis of hyperthyroidism.
If both TT4 and fT4ed are within the reference range, the patient should be evaluated further for non-thyroidal illness.
If no non-thyroidal illness is detected and the patient is still suspected to have hyperthyroidism, further testing is warranted. Options include serum TSH (thyroid stimulating hormone) in conjunction with TT4 and fT4ed, T3 suppression testing or thyroid scintigraphy. Hyperthyroid cats should have a low level of TSH.
Dynamic testing, such as the T3 suppression test, is not commonly performed in first opinion practice. The reader is directed to other texts or to contact a specialist medical centre if more information is required. Thyroid scintigraphy is a nuclear medicine procedure, where a visual display of functional thyroid tissue is produced. Calculations can be made which correlate with circulating thyroid hormone and can be used to diagnose hyperthyroidism. This would be an uncommonly recommended procedure as most patients have a diagnosis made based on blood testing.
Group 3: Cats with an enlarged thyroid gland without clinical evidence of hyperthyroidism
This group of cats have a palpable goitre, but no clinical signs of hyperthyroidism and TT4 is within the reference range. In this situation, clinical signs should be monitored and TT4 measured in six months.
Group 4: Cats with subclinical hyperthyroidism
This group of cats includes patients with an elevated TT4 and some physical examination findings suggestive of hyperthyroidism but without overt clinical hyperthyroidism. In this situation, TT4 should be re-assessed in one to two weeks. If TT4 is still elevated, the patient should be treated for hyperthyroidism. If TT4 is normal, the patient should be re-evaluated in six months with repeat TT4 assay.
Group 5: Cats with clinical hyperthyroidism and confirmed non-thyroidal disease
This group includes cats with documented concurrent disease and an elevated TT4. It is recommended to treat all cats, including those with co-morbidities. Appropriate monitoring and management of concurrent diseases will be needed.
Group 6: Cats that are clinically normal but have an elevated T4
As false elevations in TT4 can occur infrequently, it is recommended to repeat measurement. If TT4 is normal, it is recommended to monitor the patient and retest TT4 every six months or sooner. If the TT4 is elevated, treatment for hyperthyroidism is recommended.
Treatment of cats with hyperthyroidism
Medical management
Medical management is recommended initially in all cases in order to monitor the patient’s response. Where renal function remains stable, a more curative approach can then be considered. Anti-thyroid medications can be used long term also, depending on the owner’s financial situation and wishes. However, a curative treatment should be considered as there is growing evidence to suggest an increased risk of carcinomatous transformation of the thyroid adenomatous hyperplastic tissue with time.
There are several formulations of anti-thyroid drug licensed for use in Ireland. Felimazole, Dechra, is a tablet containing thiamazole (also known as methimazole), with three different strengths (1.25mg, 2.5mg and 5mg), allowing for accurate dosing. Normazole 5mg/ml and Thyronorm 5mg/ml, both Norbrook, are liquid formulations of thiamazole, again allowing for accurate dosing and offering a possibly more palatable alternative for owners. There is also a transdermal methimazole formulation manufactured by Summit Pharmaceuticals. Vidalta, Intervet Ireland, is a prolonged-release tablet containing carbimazole (a prodrug rapidly converted to the active metabolite thiamazole), which comes in two strengths (10mg and 15mg). Thiamazole acts by blocking the enzyme thyroid peroxidase, which inhibits the synthesis of thyroid hormones.
Thiamazole has a starting dose of 1.25 to 2.5mg/cat twice daily. Twice daily dosing is recommended initially. In some cases, giving the total daily dose once daily when euthyroidism has been achieved will improve compliance for some owners or patients. Starting with a higher dose once daily is discouraged, as there may be an increased risk of side effects.
Most patients achieve euthyroidism within two to three weeks after treatment is initiated. TT4 should, therefore, be measured at this time interval and thiamazole dosage adjusted based on the result. Any changes should be made in increments of 1.25-2.5mg/day until euthyroidism is achieved. It is important to discuss any compliance or administration issues with owners, as this may be the cause of lack of success. If the total required dose is in excess of 10mg/day, then an alternative treatment should be considered.
Carbimazole has a starting dose of 10mg/cat once daily. The owner should give the medication at the same time each day and either consistently with or without food. Euthyroidism may be achieved earlier in the treatment course, potentially within the first 10 days. Dosage changes should be made in increments of 5mg/day. If the total required dose is in excess of 20mg/day, then an alternative treatment should be considered.
While the response rate is high, the patients will become hyperthyroid again once medication is discontinued, a disadvantage when compared to more curative procedures. Drug reactions can occur; these include facial pruritus and gastrointestinal signs and are frequently transient, resolving within a few weeks or months. If adverse effects are persistent, therapy should be withdrawn and an alternative tried. More serious adverse effects can occur, for example, blood dyscrasias (leucopenia, anaemia, thrombocytopenia) and hepatic failure. Therefore, it is advisable to assess haematology and biochemical parameters when monitoring response to therapy.
Further disadvantages to medical management include compliance by both owner and pet and the burden on the owner to administer medication on a daily or twice daily basis. Frequent monitoring is needed initially and long-term monitoring is required to ensure continued success of therapy. As the disease progresses, the dosage of medication may need to be increased. The adenomatous tissue continues to hypertrophy and secrete thyroid hormones. There is evidence that the risk for carcinomatous transformation increases as the treatment period increases, therefore increasing the risk of malignancy for patients that are diagnosed while younger.
Radioactive iodine
Radioactive iodine (RAI) is generally regarded as the gold standard treatment choice for hyperthyroidism in stable patients. In Ireland, it is only available at University College Dublin. It may be unsuitable for patients with significant comorbidities or for patients that are particularly fractious. It has a 95 per cent cure rate from a single subcutaneous injection of radioactive isotope, Iodine-131 (131I). It has the advantages of controlling disease in functional extrathyroidal tissue, which may occur in 10 to 20 per cent of hyperthyroid cats. No general anaesthesia is required for administration.
Medical management of hyperthyroidism is recommended initially, in order to monitor the patient’s response to therapy and to monitor for any alterations in renal function. In the weeks before RAI treatment, medical management is discontinued to allow abnormal tissue to become functional again and allow uptake of the radioactive isotope.
After administration, the thyroid gland concentrates the radioactive iodine, which emits radiation. The radioactive particles destroy thyroid tissue, but have a limited range of 2mm. Therefore, there is no significant damage to the adjacent parathyroid gland or other cervical structures.
The iodine that is not concentrated in the thyroid gland is rapidly eliminated in the urine, saliva and sweat in the first couple of days following the injection. The remainder is slowly eliminated due to thyroid hormone turnover (with the 131I incorporated into the hormone) and due to decay of the isotope (the half-life of 131I is eight days). Therefore, cats must stay in an isolation facility until most of the radioactivity has been eliminated.
Following discharge from the clinic, cats are typically represented to the primary practice at three and six months post 131I injection, or sooner, if concurrent disease is present or has been detected during hospitalisation. At these checks, the patient requires a full examination, including weight check and blood and urine sampling.
If the TT4 is found to be low at the three-month check and creatinine is <140umol/l, no further investigation is required at that time. If the patient is azotaemic with a USG < 1.035, then measurement of TSH is recommended. If this is normal, reassessment will proceed at the six-month check. If TSH > 0.15ng/ml, levothyroxine supplementation may be required (generally 100ug/cat twice daily, or 150ug/cat once a day, although it would be advisable to discuss this first with the radioactive iodine clinic).
If the TT4 is found to be low at the six-month check, TSH should be measured. If TSH is normal, no treatment is required. If TSH is >0.15ng/ml and creatinine is <140umol/l, thyroid hormone supplementation can be considered, particularly for cats who have clinical signs of hypothyroidism (for example, excessive weight gain, dullness, lethargy). For cats with elevated TSH and evidence of azotaemia or USG <1.035, levothyroxine supplementation is needed. Total T4 and renal function should be reassessed one month following treatment initiation, four to six hours following supplementation. Dosage should be altered based on results and re-testing performed again after one month. Long term, thyroid function should be assessed one or two times per year as a minimum, along with the recommended renal function monitoring per IRIS (International Renal Interest Society) guidelines.
Surgical thyroidectomy
There are several surgical options, including unilateral or bilateral thyroidectomy with an intracapsular, extracapsular or modified extracapsular approach. Importantly, there is a morbidity and mortality associated with these procedures. General anaesthetic risk must be considered. Hypocalcaemia can occur as a result of parathyroid damage or inadvertent removal causing hypoparathyroidism and this may be transient or permanent. Laryngeal nerve paralysis, Horner’s syndrome, infection or haemorrhage can also occur. It is important to remember that a small proportion of cats have ectopic adenomatous tissue (sublingual or substernal locations are most common). Hyperthyroidism may recur if any ectopic thyroid tissue remains, if tissue is left behind due to surgical technique or if a unilateral thyroidectomy is performed.
Surgical treatment of hyperthyroidism has a high rate of success with over 90 per cent of patients achieving euthyroidism. There is an approximate relapse rate of five per cent within three years following surgery. Transient hypothyroidism may occur with a unilateral thyroidectomy as the remaining thyroid gland may take one to three months to recover function. Bilateral thyroidectomies can result in a permanent clinical hypothyroidism requiring hormone replacement.
Dietary therapy
Limiting dietary iodine intake has been used to control thyroid hormone production. This needs to be the only food given to the patient and around 75 per cent of cats have a reduced TT4 and improvement of clinical signs within 28 days of starting the diet. Euthyroidism can be delayed or never achieved in cats with severe elevations in TT4.
Lack of palatability and compliance are common issues. For cats with concurrent issues requiring dietary management, for example CKD, this method of thyroid control is not possible. Environmental factors, such as multi-cat households and hyperthyroid cats that go out, also need to be considered.

Table 4.
Treatment of cats with hyperthyroidism and comorbidities
Hyperthyroidism and CKD
The evidence supports a rationale to treat hyperthyroidism while avoiding hypothyroidism in patients with concurrent CKD. Iatrogenic hypothyroidism has been shown to have a deleterious effect on renal function if maintained in this state.
Treatment is recommended for cats with pre-existing azotaemia and those who develop azotaemia during treatment. The ‘old wives tale’ of keeping cats a little bit hyperthyroid to maintain renal perfusion is a misconception. This approach will likely increase renal damage long term, due to persistent activation of the renal-angiotensin-aldosterone system. For cats that develop azotaemia during treatment, it has been shown that these patients generally have a poorer prognosis long-term.
The Guidelines recommend treating IRIS Stage 1 and 2 patients as if they are non-azotaemic. If the patient’s renal function remains stable when using a reversible hyperthyroid treatment, it is then possible to consider an irreversible hyperthyroid treatment.
IRIS Stage 3 and 4 CKD patients with hyperthyroidism require a more pragmatic and cautious approach. Lower doses of medication may be required to balance euthyroidism and active management of CKD should be pursued. In cats with CKD, some clinicians recommend maintaining a serum T4 in the upper half of the reference interval. This reduces the risk of periods of hypothyroidism.
Hyperthyroidism and concurrent cardiac disease
Cardiac disease is a common finding in hyperthyroid patients and may or may not be caused by the hyperthyroid state. Further evaluation of patients is generally recommended. An echocardiogram provides the most information on cardiac size and function. An electrocardiogram is appropriate when an arrhythmia is auscultated or when the clinician wants to make a complete assessment.
Patients may infrequently present in congestive heart failure and concurrent hyperthyroidism. There is also the potential for patients with hyperthyroidism to initially present with a feline arterial thromboembolism.
Treatment of cats who develop hypothyroidism
Patients may develop iatrogenic hypothyroidism as a result of treatment of hyperthyroidism. Where this has occurred due to a reversible treatment, then modification of medication and subsequent rechecking of TT4 should be implemented to revert to euthyroidism. Where this has occurred due to radioactive iodine therapy or thyroidectomy, hormone supplementation may be required.
Typically, the thyroxine nadir occurs two weeks after radioiodine treatment, with TT4 normalisation occurring around four weeks after treatment. Supplementation with levothyroxine during this period will resolve iatrogenic hypothyroidism and may be necessary in clinically hypothyroid patients. However, this treatment will also suppress pituitary TSH, which is needed to stimulate regeneration of atrophied thyroid tissue.
The evaluation of creatinine, T4 and TSH tests may help to determine whether T4 supplementation is necessary (see earlier in this article under “Treatment of cats with hyperthyroidism”).
Monitoring of hyperthyroid cats, long term
Following implementation of treatment, it is recommended to reassess the patient at two to four weeks. Total T4 measurement should be performed at this check and at two to four weeks after any dosage change. If patients are stable and uncomplicated by concurrent disease, cats can be monitored every four to six months. Patients with concurrent disease may require more frequent re-evaluations. For patients treated with radioactive iodine, if the patient achieves euthyroidism after appropriate monitoring (see under “Treatment of cats with hyperthyroidism”), routine monitoring only is generally necessary. For cats undergoing thyroidectomy, monitoring for the recurrence of hyperthyroidism is required.
Bree, L. et al (2018) Prevalence and risk factors for hyperthyroidism in Irish cats from the greater Dublin area. Irish Veterinary Journal, 71:2, https://doi.org/10.1186/s13620-017-0113-x
Carney, H.C. et al (2016) 2016 AAFP Guidelines for the Management of Feline Hyperthyroidism. Journal of Feline Medicine and Surgery, 18, pp.400-416.
Taylor, S.S. et al (2017) ISFM Consensus Guidelines on the Diagnosis and Management of Hypertension in Cats. Journal of Feline Medicine and Surgery 19, pp.288-303.
1. If the following abnormality is seen alongside an elevated TT4, the patient should be assessed for concurrent disease:
A. Elevated ALKP
b. Elevated ALT
C. Erythrocytosis
D. Anaemia
2. Functional extrathyroidal tissue can occur in what percentage of cats:
A. 10-20
b. 1-2
C. 50-60
D. 25-30
3. The following adverse drug reaction is not seen with anti-thyroidal medication administration:
A. Facial pruritis
b. Kidney failure
C. Liver failure
D. Vomiting
4. Radioactive iodine is effective in curing what percentage of hyperthyroid cats with a single subcutaneous injection:
A. >95
b. >50
C. >65
D. >80
5. The following is not a common clinical sign associated with hyperthyroidism:
A. Vomiting
b. Weight loss
C. Polyphagia
D. Anorexia
ANSWERS: 1D; 2A; 3B; 4A; 5D.














