Treating brachycephalic obesity in Ireland: an RVN approach to tackling the challenges that arise
Michelle Tobin RVN analyses the results of a survey she carried out to assess the effectiveness of weight management interventions by RVNs in the treatment of brachycephalic obesity in Ireland
Brachycephalic obesity is a major concern due to its exacerbating effect on Brachycephalic Obstructive Airway Syndrome (BOAS). Affected animals suffer from hypoplastic airways, resulting in dyspnoea, sleep disorders, increased risk of laryngeal and tracheal collapse, increased risk of choking, exercise intolerance and overall reduced quality of life. Weight loss has been shown to alleviate clinical signs of BOAS in affected breeds, therefore, Irish RVN-led weight management interventions were evaluated to determine whether they are successful.
This article reports on a survey of RVNs with experience working in companion animal practice in Ireland, which sought to determine the effectiveness of weight management interventions. The results showed that RVNs often encounter many issues when attempting to treat the obese brachycephalic dog, including client co-operation factors and patient co-morbidities. It was discovered that there is a perception amongst RVNs that clients are the primary challenge that they contend with when attempting to treat their brachycephalic pets’ obesity. However, most RVNs also lack confidence, either in themselves and/or in their practices, to effectively manage brachycephalic obesity. Negative client perceptions could be resulting in conflict between the client and the veterinary professional.
These issues could theoretically be solved through further training, a tailored approach to suit individual clients, and patients, as well as an increased level of patience and understanding on the part of the RVN.
Introduction
Companion animal obesity rates are increasing in Western countries (German, 2006), and Ireland is no exception, despite the high standard of veterinary care available. The root causes for companion animal obesity are complex; humans have sole control over the diets of their pets to prevent or reverse obesity and yet, obesity levels are continuing to rise.
There are several definitions used to measure obesity, but it is commonly defined as the accumulation of excessive bodyweight of 30 per cent above optimal (Schmalberg, 2013) or a Body Condition Score (BCS) of between 5/9 (Packer & Tivers, 2015) and 7/9 (Ladlow et al, 2018). Blood plasma markers for chronic inflammation show that metabolically active adipose tissue releases hormones and cytokines into the body, resulting in a state of chronic, low-grade inflammation and hypercoagulopathy (Rafaj et al, 2017). This is associated with many serious health concerns including increased insulin sensitivity and the propensity to develop blood clots (German et al, 2012), among other issues that negatively impact the quality of life (QOL) of affected animals.
Designated RVN-led clinics are now being offered to clients in many small and mixed animal veterinary practices across Ireland and the UK (Ackerman, 2015). Regardless of whether RVNs engage with active nursing clinics in practice, many RVNs have at least some experience advising clients on their pets’ weight. The RVN is often tasked by the veterinary practitioner (VP) with creating individualised weight management plans for obese pets using a combination of various strategies aimed at helping patients to decrease calorie consumption while increasing activity levels, culminating in a caloric deficit, resulting in weight loss. What is unknown, however, is whether these weight loss interventions are successful at reducing the rates of obesity in Ireland. The purpose of the research focused on in this article was to conduct an exploratory investigation into evaluating the efficacy of Irish RVN-led weight loss techniques, with a particular focus on the treatment of canine brachycephalic patients.
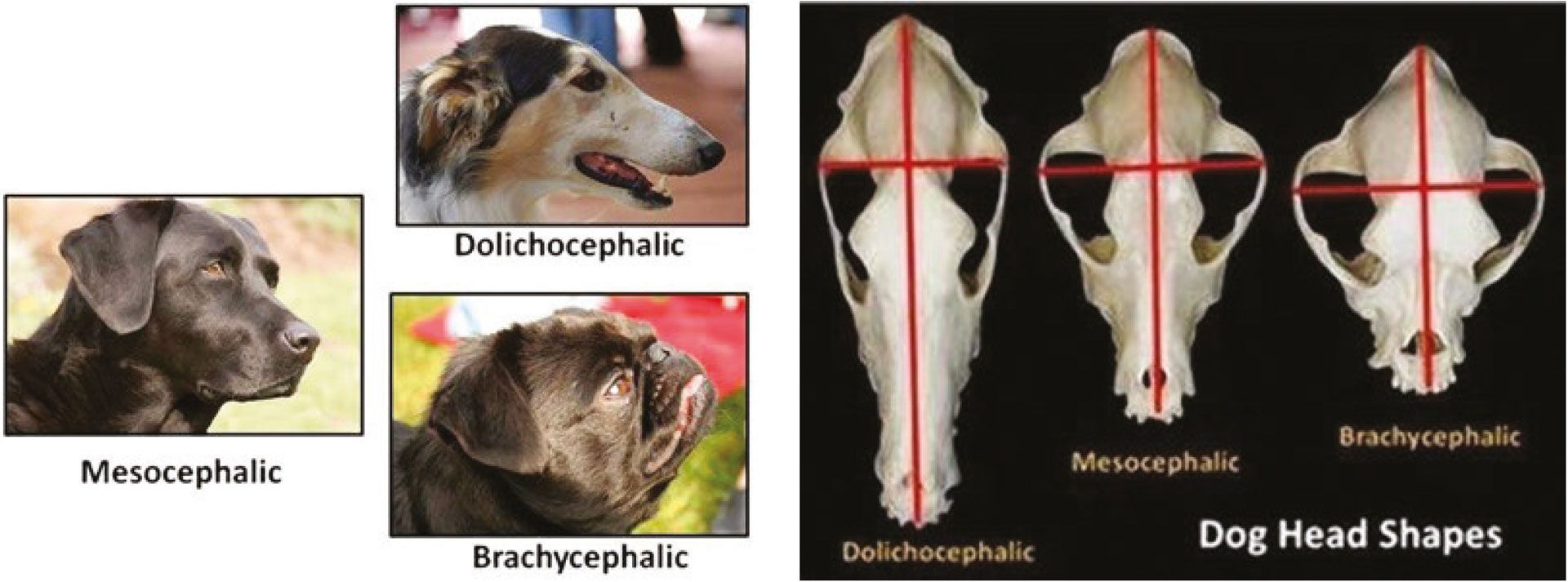
Figure 1.1 and 1.2: Three different skull types (Coren, 2021).
Brachycephalic conformation and comparative anatomy
There are three different canine skull types (Figures 1.1 and 1.2): doliocephalic, mesocephalic and brachycephalic. Doliocephalic skulls are the longest skull type and are characterised by a cranial length that is much greater than the cranial width. Breeds with this skull type, such as greyhounds and whippets, often have a higher range of vision due to optimal eye position on a long and narrow snout. The mesocephalic skull is more proportional, in that the length and width of the cranium is more similar in measurement. These breeds, including Labrador retrievers and cocker spaniels, have broad snouts and nasal passages, increasing their sense of smell. Brachycephalic skulls are regarded as where the cranial width is at least 80 per cent of the length. Affected breeds, some of which include French bulldogs, English bulldogs and pugs have very short snouts, resulting in reduced nasal passage capacity; this affects breathing capability, and increases overheating due to the insufficiency of the nasal passages to filter and cool air (Khan, 2015).
Brachycephalic dog breeds are of particular concern where they are also affected by obesity due to the negative impact of excess fat on their compromised airways due to a craniofacial malformation (Figure 2). In dogs bred for brachycephalic phenotypic features, the tracheal and laryngeal cartilages develop abnormally, resulting in them becoming hypoplastic, or narrowed. Excessive weight gain can further constrict already narrowed airways, leading to dyspnoea, sleep disorders, and exercise intolerance. Obesity has been shown to exacerbate clinical signs of the genetic disorder Brachycephalic Obstructive Airway Syndrome (BOAS) (Philips & Jaeger, 2016) which results in chronic suffering and reduces their overall longevity (German et al, 2012).
Accumulation of adipose tissue in the throat can further compound the narrowing that already exists in brachycephalic breeds, which can eventually lead to complete tracheal and/or laryngeal collapse, which is fatal without rapid veterinary intervention. The soft palate is anatomically elongated and thickened in brachycephalic animals, exposing affected breeds to potential obstructions, and increasing the risk of choking.
Obesity also exacerbates soft palate tissue thickening by accumulating fat cells in this area, further increasing the choking risk. The nares are stenotic, meaning that nasal passages are narrowed, reducing the ability of affected breeds to breathe through their nose. Nasal turbinates often deviate rostrally in brachycephalic animals, meaning that they are less branched, impairing the ability to inspire and filter air. Furthermore, the compressed caudal turbinates protrude into the naso-pharynx which impacts negatively upon the passage of air from the nose to the lungs and increases the risk of infections. Again, the fat deposits resulting from obesity constrict these passageways even further and intensify the problems that are already apparent in brachycephalic breeds, increasing their overall risk of disease and ultimately reducing their QOL (Cambridge Veterinary School, 2021).
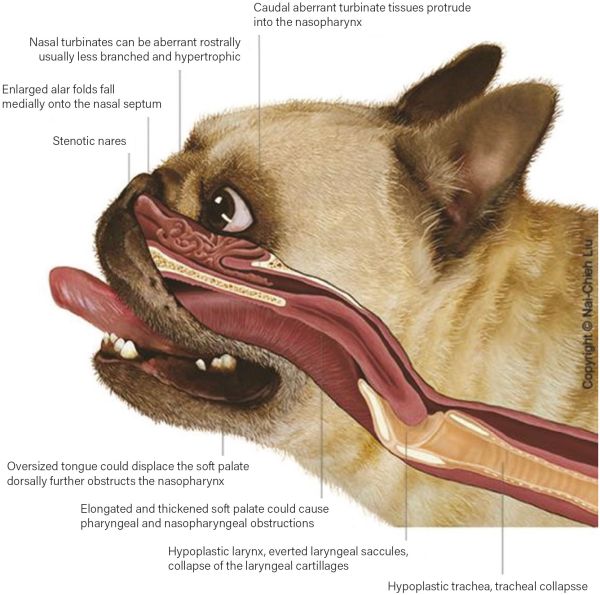
Figure 2: Canine Brachycephalic Anatomy (Cambridge Veterinary School, 2021).
Literature review
Brachycephalic dogs are often affected by a multitude of negative health issues, collectively referred to as a condition called ‘Brachycephalic Obstructive Airway Syndrome’ (BOAS). Anatomically, BOAS often presents as an elongated soft palate, everted laryngeal saccules, and stenotic nares. The consequences of this include marked respiratory noise, dyspnoea, exercise intolerance, heat sensitivity, sleep disorders, cyanosis, or collapse (Philips & Jaeger, 2016). BOAS is a progressive disease, according to one study which noted severe respiratory signs and exercise intolerance in pugs and French Bulldogs (Roedler et al, 2013).
Limited research studies suggest a significant correlation between obesity and exacerbation of the negative effects of BOAS (Liu et al, 2015), (Packer et al, 2015) as the accumulation of adipose tissue in the airway tract can further narrow the lumen, compounding the breathing restriction that BOAS-affected animals already have regardless of BCS (Cambridge Veterinary School, 2021). In one study, it was found that obese dogs are reported to be 1.9-fold more likely than dogs with a normal BCS to show signs of BOAS (Tarricone et al, 2019).
In a study carried out in China, it was discovered that more than 44 per cent of the dogs presented to veterinary hospitals were obese, with pugs having the highest obesity prevalence rate of 70 per cent, according to the BCS scoring chart (Mao et al, 2013). Similarly in a UK study, 80 per cent of pugs intended for show were classified as overweight or obese (Such & German, 2015).
Other research conducted in the UK reported 50 per cent obesity rates for pugs and French Bulldogs and 45 per cent for English Bulldogs. Although these rates do not represent the Irish brachycephalic population, it can be theorised that obesity rates would be similar here.
Optimistically, the research also indicates that maintaining a normal bodyweight can help to alleviate clinical signs associated with the condition, such as improvement in airway function (Ladlow et al, 2018), as well as increasing general longevity (German et al, 2012). One study found that French Bulldogs with a lower BCS were less affected by BOAS (Liu et al, 2016). Within the existing limited knowledge base on brachycephalic obesity, it can be extrapolated and concluded that weight loss does improve the QOL of brachycephalic dogs and alleviate suffering caused by BOAS-related co-morbidities (Yam et al, 2016).
There is extremely limited research available on the evaluation of RVN weight management interventions, generally. However, in one Australian study on weight loss clinics, veterinary practices believed that just three per cent of obesity cases could be attributed to dog-specific factors and 97 per cent to human factors including diet, exercise, and owner attitudes (Bland et al, 2010). What this research does not address, is the unique implication that obesity has on brachycephalic dog breeds specifically. In the same study, it was found that 43 per cent of practices in Victoria ran designated obesity clinics with 79 per cent of these practices believing them to be effective. Conversely, of the practices that did not run clinics, just 46 per cent believed them to be effective (Bland et al, 2010). It would be extremely useful to have comparable data in the Irish context, but there are currently no research studies in Ireland seeking to assess the effectiveness of weight management clinics or general interventions.
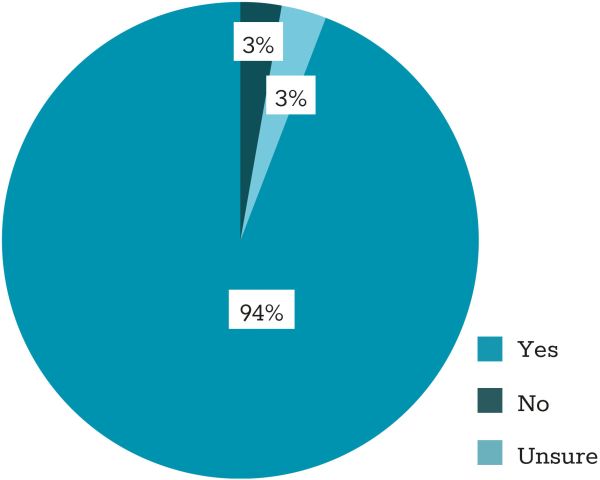
Figure 3: Is there any association between obesity and BOAS?
Results
Demographics
There were 52 respondents to the survey, of which 35 met the eligibility criteria and were authorised to proceed (67.3 per cent). Of these, the majority had been working in small animal practice for between one and five years (51.4 per cent), followed by 22.8 per cent having worked for five to 10 years.
Survey findings
It was found that most respondents use a combination of BCS scoring and scale weight to diagnose obesity in their patients. A small number of respondents use measurements (31.4 per cent), however, the implementation of measurements in the overall approach to obesity diagnosis may be useful to use in conjunction with other techniques especially as there can be huge variation in body proportions across different canine breeds. Most respondents cite no greater than 60 per cent of breeds attending the practice for weight loss purposes are brachycephalics. While 94 per cent of respondents acknowledge an association between obesity and BOAS, 5.7 per cent either disagree or are unsure that there is a connection between them (Figure 4).
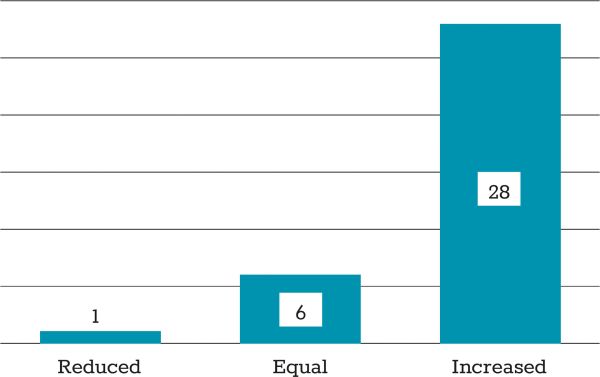
Figure 4: Are brachycephalic breeds at a reduced, equal or increased risk of obesity, compared to the standard dog population?
Almost 20 per cent of respondents cite brachycephalics as being at a reduced or equal risk of obesity compared to the mesocephalic population (Figure 4), despite it being reported in the existing literature that one major clinical sign indicating implications of BOAS is exercise intolerance (Liu et al, 2015), (Packer et al, 2015).
When asked to rate brachycephalic obesity control priority on a scale of one to five (one being lowest priority and five being highest priority), the average response was 2.94/5, or a 59 per cent priority rate. It is interesting to note that 17.1 per cent of respondents either disagree or are unsure that there are any extra considerations to factor into a weight loss plan for a brachycephalic dog, despite these breeds being at increased risk of BOAS which often causes dyspnoea, GI issues, exercise intolerance and obesity (Philips & Jaeger, 2016).
Of the 27/35 respondents who agreed that extra considerations needed to be taken into account for a brachycephalic patient’s weight loss plan, exercise was cited as the main factor to consider (Figure 5). This is supported by the existing literature on the topic, as severe respiratory signs in conjunction with exercise intolerance have been noted in French Bulldogs and pugs (Roedler et al, 2013). This ties in with general BOAS-related issues and the potential for certain types of exercise to exacerbate BOAS. It is interesting that exercise and BOAS factors combined are cited the most here (85.2 per cent of responses), as opposed to owner factors (29.6 per cent), which features in RVN responses more prominently in later questions.
Respondents were asked to rate their practice’s success rate at getting mesocephalic and brachycephalic dogs, respectively, to lose weight. Respondents reported an 11.4 per cent higher success rate of mesocephalic weight loss reduction as opposed to brachycephalic weight loss reduction (Table 1).
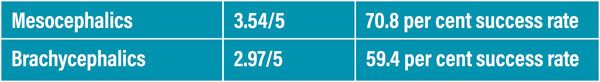
Table 1: Weight loss success rates for mesocephalic Vs brachycephalic dogs.
All respondents in the survey cited client co-operation as being one of the major challenges to addressing obesity concerns in the brachycephalic dog. It is encouraging that 60 per cent of respondents cite co-morbidities as the second highest challenge as it acknowledges the difficulties that present to treat the obese brachycephalic patient because of their disorder and concurrent conditions. It is important to note that just 11.4 per cent of respondents cite a need for more training; a point that will be discussed further on in more detail.
A question on owner-specific characteristics contributing to weight loss challenges yielded 26 responses. Main themes include: the desire for specific physical attributes, lack of owner education, spoiling, non-co-operation, and a ‘normal for the breed’ mentality. It is clear from the results shown that an emphasis on owner education focused on obesity prevention may be key for treating obesity in these breeds (Figure 6).
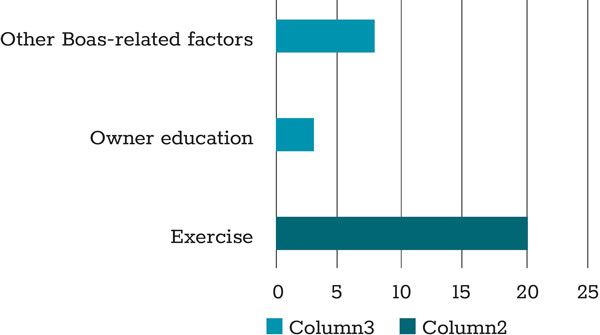
Figure 5: Brachycephalic weight loss considerations.
All respondents in the survey cited client co-operation as being one of the major challenges to addressing obesity concerns in the brachycephalic dog. It is encouraging that 60 per cent of respondents cite co-morbidities as the second highest challenge as it acknowledges the difficulties that present to treat the obese brachycephalic patient because of their disorder and concurrent conditions. It is important to note that just 11.4 per cent of respondents cite a need for more training; a point that will be discussed further on in more detail.
A question on owner-specific characteristics contributing to weight loss challenges yielded 26 responses. Main themes include: the desire for specific physical attributes, lack of owner education, spoiling, non-co-operation, and a ‘normal for the breed’ mentality. It is clear from the results shown that an emphasis on owner education focused on obesity prevention may be key for treating obesity in these breeds (Figure 6).
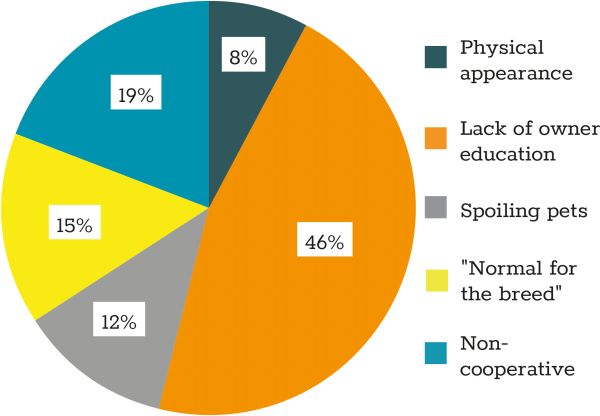
Figure 6: Owner characteristics contributing to weight loss challenges.
Survey participants were asked about confidence in their ability to give good weight loss advice to owners of brachycephalic dogs. In the second-last question about the ‘challenges to addressing weight issues in the brachycephalic dog’, 11.4 per cent of respondents cited a need for more training/CPD, yet in this question, only 34.29 per cent of respondents were confident in their ability to give good weight loss advice, whereas 65.76 per cent were either not confident or felt as though there was room for improvement (Figure 7).
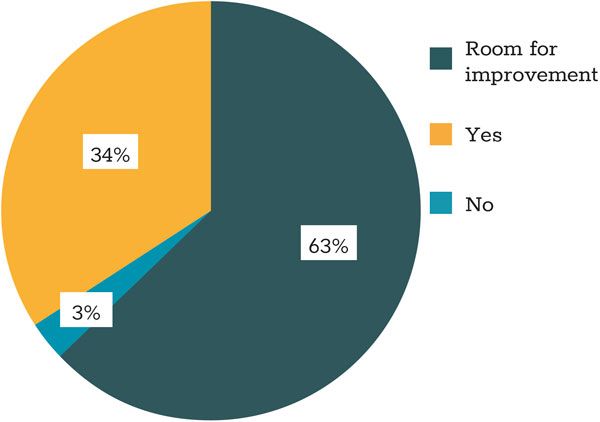
Figure 7: Are you confident in your ability to give good weight loss advice to owners of brachycephalic dogs?
In a similar vein to the last point made, just 14.23 per cent of respondents think that their clinic’s weight management interventions are effective, while a comparatively high 85.7 per cent either disagree that they are effective or cite room for improvement. It is notable that most of the responsibility seems to be placed on the client for their pet’s obesity and the treatment of it, however, these statistics highlight an issue within the veterinary practice itself and the effectiveness of their weight management interventions.
When asked to give advice to other RVNs regarding approaches to tackling brachycephalic obesity, the primary focus was on owner education and co-operation (49 per cent). The cohesiveness of the veterinary team was also deemed to be of particular importance (25 per cent), while research and perseverance were other themes that arose in the survey responses (Figure 8).
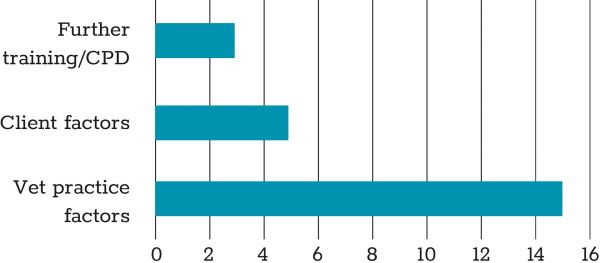
Figure 8: General suggestions to help improve RVN weight management clinics.
Overall, 85.7 per cent of respondents who run weight clinics believe that RVN-led weight management clinics are effective. This result is comparable to, and even more positive, than the Australian study that rated the success of their RVN-led weight management clinics at 79 per cent (Bland et al, 2010). It is encouraging to see that most respondents believe that veterinary nurse-led weight management clinics work.
Summary of key findings
Key finding 1
Client co-operation was cited by 100 per cent of respondents to be one of the major challenges behind treating brachycephalic obesity.
Key finding 2
RVNs often lack the confidence in themselves and/or their practice in terms of providing sound weight management advice. This is an important point for RVNs to note because it takes the emphasis off the client and places responsibility back with the RVN. Self-evaluation and identification of specific areas of improvement can help the RVN equip themselves with the knowledge, skill and confidence required to implement tailored brachycephalic weight management plans. Further training, engagement with CPD and shadowing more experienced RVNs can all contribute towards overall improvement in this area (Wild, 2017).
Key finding 3
Patient co-morbidities are a major causal factor for the development of brachycephalic obesity. Concerns regarding the ability to exercise was overwhelmingly expressed through the responses.
Conclusion
The results of the survey demonstrated that although brachycephalic obesity can be difficult to treat with RVN interventions, it is most likely to be effective when the client and veterinary professional can form a good relationship and work well together to follow through with a specific plan.
Client education is at the core of finding a solution to the challenges of treating brachycephalic obesity. RVNs are key to addressing any tension or conflict between the client and the veterinary professional; it is vital to ensure that messages between the client and veterinary professional regarding the patient are conveyed and received clearly and free from ambiguity. The RVN may need to employ an attitude of increased patience and understanding with perceived challenging clients to maintain a good working relationship with them.
Despite the obvious co-morbidities associated with BOAS-affected dogs, RVN weight management interventions have greater chances of success when implemented as part of a strong client education plan by confident, calm, patient RVNs who have received sufficient training in this area.
- Ackerman, N., 2015. Setting up veterinary nurse. In Practice, Volume 37, pp. 199-202.
- Bland, I. M., Guthrie-Jones, A., Taylor, R. D. & Hill, J., 2010. Dog obesity: veterinary practices’ and owners’ opinions on cause and management. Preventive Veterinary Medicine, 94(1-4), pp. 310-315.
- Bree, R. & Gallagher, G., 2016. Using Microsoft Excel to code and thematically analyse qualitative data: a simple, cost-effective approach. AISHE-J, 8(2), pp. 2811-28114.
- Cadogan, S., 2021. Ireland has a record number of veterinary professionals. [Online] Available at: https://www.irishexaminer.com/farming/arid-40208150.html
- [Accessed 21 November 2021]
- Cambridge Veterinary School, 2021. Pathophysiology of BOAS. [Online] Available at: https://www.vet.cam.ac.uk/boas/about-boas/pathophysiology
- [Accessed 21 November 2021]
- Centers for Disease Control and Prevention, 2022. One Health Basics. [Online]
- Available at: https://www.cdc.gov/onehealth/basics/index.html
- [Accessed 07 April 2022]
- Coren, S., 2021. Why Many People Love Snub-Nosed Dogs: It’s Those Eyes. [Online]
- Available at: https://www.psychologytoday.com/ie/blog/canine-corner/202105/why-many-people- love-snub-nosed-dogs-its-those-eyes
- [Accessed 29 04 2022]
- Fasanella, F. J., Shivley, J. M., Wardlaw, J. M. & Givaruangsawat, S., 2010. Brachycephalic airway obstructive syndrome in dogs: 90 cases (1991–2008). Journal of the American Veterinary Medical Association, 237(9), pp. 1048-1051.
- German, A. J., 2006. The Growing Problem of Obesity in Dogs and Cats. The Journal of Nutrition,
- 136(7), pp. 1940-1946.
- German, A. J. et al, 2012. Quality of life is reduced in obese dogs but improves after successful weight loss. Veterinary Journal , 192(3), pp. 428-434.
- Irish Statute Book, 2021. Veterinary Practice Act 2005. [Online]
- Available at: https://www.irishstatutebook.ie/eli/2005/act/22/enacted/en/html
- [Accessed 22 November 2021]
- Khan, A., 2015. It’s all in the head - A detailed insight into Dog Skulls. [Online]
- Available at: https://www.dogspot.in/dog-blog/its-all-in-the-head-a-detailed-insight-into-dog-skulls/
- [Accessed 29 04 2022]
- Ladlow, J., Liu, N.-C., Kalmar, L. & Sargan, D., 2018. Brachycephalic obstructive airway syndrome. The Veterinary Record, 182(13), pp. 375-378.
- Lilja-Maula, L. et al, 2017. Comparison of submaximal exercise test results and severity of brachycephalic obstructive airway syndrome in English bulldogs. The Veterinary Journal, Volume 219, pp. 22-26.
- Liu , N. C., Sargan, D. R., Adams , V. J. & Ladlow , J. F., 2015. Characterisation of Brachycephalic Obstructive Airway Syndrome in French Bulldogs Using Whole-Body Barometric Plethysmography. Plos One, 10(6).
- Liu, N. C., Adams, V. J., Kalmar, L. & Sargan, D. R., 2016. Whole-Body Barometric Plethysmography Characterizes Upper Airway Obstruction in 3 Brachycephalic Breeds of Dogs. Journal of Veterinary Internal Medicine, 30(3), pp. 853-865.
- Maguire, M. & Delahunt, B., 2017. Doing a Thematic Analysis: A Practical, Step-by-Step. AISHE-J,
- Issue 3, pp. 3351-33514.
- Mao, J., Xia, Z., Chen, J. & Yu, J., 2013. Prevalence and risk factors for canine obesity surveyed in veterinary practices in Beijing, China. Preventive Veterinary Medicine, 112(3-4), pp. 438-442.
- McCombs, S., 2020. Scribbr: How to write a methodology. [Online] Available at: https://www.scribbr.co.uk/thesis-dissertation/methodology/ [Accessed 09 December 2021]
- Meyers, L., 2014. Connecting with clients. [Online]
- Available at: https://ct.counseling.org/2014/08/connecting-with-clients/
- [Accessed 10 04 2022]
- Packer, R., Hendricks, A. & Burn, C., 2012. Do dog owners perceive the clinical signs related to conformational inherited disorders as ‘normal’ for the breed? A potential constraint to improving canine welfare. Animal Welfare, 21(1), pp. 81-93.
- Packer, R., Hendricks, A., Tivers, M. & Burn, C., 2015. Impact of Facial Conformation on Canine Health: Brachycephalic Obstructive Airway Syndrome. PLoS One, 10(10).
- Packer, R. M. & Tivers, M. S., 2015. Strategies for the management and prevention of conformation- related respiratory disorders in brachycephalic dogs. Vet Med (Auckl), Volume 6, pp. 219-232.
- Philips, H. & Jaeger, M., 2016. Brachycephalic Syndrome. Veterinary Team Brief, Issue September,
- pp. 31-37.
- Rafaj, R. B. et al, 2017. Plasma markers of inflammation and hemostatic and endothelial activity in naturally overweight and obese dogs. BMC Veterinary Research, 13(13), pp. 1-7.
- Riggs, J. et al, 2019. Validation of exercise testing and laryngeal auscultation for grading brachycephalic obstructive airway syndrome in pugs, French bulldogs, and English bulldogs by using whole-body barometric plethysmography. Veterinary Surgery, 48(4).
- Roedler, F. S., Pohl, S. & Oechtering, G. U., 2013. How does severe brachycephaly affect dog’s lives? Results of a structured preoperative owner questionnaire. The Veterinary Journal, 198(3), pp. 606- 610.
- Schmalberg, J., 2013. Treatment of Obesity: Current Research & Recommendations. Today’s Veterinary Practice, pp. 60-65.
- Such, Z. R. & German, A. J., 2015. Best in show but not best shape: a photographic assessment of show dog body condition. The Veterinary Record, 177(5).
- Tarricone, J., Hayes, G. M., Singh, A. & Davis, G., 2019. Development and validation of a brachycephalic risk (BRisk) score to predict the risk of complications in dogs presenting for surgical treatment of brachycephalic obstructive airway syndrome. Veterinary Surgery, 48(7), pp. 1253-1261.
- Wild, S., 2017. Veterinary nurse clinics – opportunities and obstacles. Veterinary Nursing Journal,
- 32(4), pp. 118-120.
- Yam, P. S. et al, 2016. Impact of canine overweight and obesity on health-related quality of life.
- Preventative Veterinary medicine, Volume 127, pp. 64-69.
The cranial width of brachycephalic skulls is at least what percentage of the cranial length?
A. 60 per cent
B. 70 per cent
C. 80 per cent
D. 90 per cent
2. What effects does obesity have on an animal?
A. Chronic inflammation as a result of metabolically active adipose tissue releasing hormones and cytokines into the body.
B. Hypocoagulopathy of the blood resulting in decreased insulin sensitivity and potential for haemorrhage.
C. Negative quality of life, but normal life span.
D. Increased energy due to calorie overload.
3. Which of the following groups detailing clinical signs of Brachycephalic Obstructive Airway Syndrome are correct?
A. Sleep disturbances, shortened soft palate, exercise intolerance, gastrointestinal disorders.
B. Stertor and stridor, everted laryngeal saccules, normal dental occlusion, obesity in the breed.
C. Cold intolerance, dysphagia, ocular disorders, deviated nasal turbinates.
D. Dyspnoea, stenotic nares, hypoplastic trachea and larynx, thickened soft palate.
4. What percentage of Irish RVNs are self-confident in brachycephalic weight management consultations?
A. 8 per cent
B. 34 per cent
C. 66 per cent
D. 79 per cent
5. How can RVNs strive for better weight loss outcomes in brachycephalic patients?
A. Explain to the owner that the patient requires a strict feeding and exercise regime.
B. Work closely with the client to design a plan with their input to ensure that weight management recommendations can be implemented at home.
C. Recommend that the owner schedule a consultation with the veterinary practitioner if there is a personality clash.
D. Improve self-confidence by engaging with further training and CPD courses surrounding obesity and brachycephalic animals.
ANSWERS: 1C; 2A; 3D; 4B; 5B and D.















