Inflammatory diseases of the CNS in dogs
Non-infectious inflammatory diseases affecting the central nervous system (CNS)are a frequent neurological presentation in both first-opinion and referral practice. Sarah Butterfield BSc(Hons) BVSc PGDip(VCP) MRCVS, Resident in Neurology and Neurosurgery, Queen Mother Hospital for Animals (RVC London), provides a brief overview of the most common specific clinical syndromes and how these can be treated
Inflammation affecting the central nervous system is a common cause of neurological signs with non-infectious (suspected immune-mediated) disease much more common than infectious disease in dogs in England, affecting 83.6 per cent compared to 16.4 per cent respectively in one study. Many non-infectious meningoencephalomyelitides (NIME) have been described including steroid-responsive-meningitis-arteritis (SRMA) and meningoencephalitis of unknown aetiology (MUA), as well as corticosteroid-responsive tremor syndrome (CRTS), idiopathic hypertrophic pachymeningitis and eosinophilic meningoencephalitis. Histologically, MUA can be categorised into granulomatous meningoencephalitis (GME), necrotising meningoencephalitis (NME) and necrotising leucoencephalitis (NLE). When the spinal cord is affected the term ‘myelitis’ may be used.
Signalment and clinical presentation differ between disease process and so can help generate a likely list of differential diagnoses. In all inflammatory conditions, neurological signs are typically acute in onset and progressive. Prognosis is variable and dependent on disease process, extent of CNS involvement and response to treatment. Given the suspected immune-mediated aetiology with such conditions, treatment is usually immuno-suppressive doses of corticosteroids, often in combination with a second immuno-modulatory drug.
Steroid-responsive meningitis-arteritis (SRMA)
SRMA, previously known as Beagle pain syndrome, necrotising vasculitis, aseptic suppurative meningitis and others, causes diffuse inflammation of the leptomeninges and associated small blood vessels. A recent, detailed review of the condition has been published in the Veterinary Ireland Journal in November 2021.
Signalment: Dogs affected are typically young (six to 18 months old) and predisposed breeds include Beagles, Boxers and Bernese Mountain Dogs, as well as German Shorthaired Pointers and Nova Scotia Duck-Tolling Retrievers.
Presentation: Clinical signs include general malaise, pyrexia, reluctance to walk, low neck carriage (see Figure 1) and hunched posture. As the disease process affects the leptomeninges rather than spinal cord parenchyma, dogs are typically neurologically normal with marked cervical hyperaesthesia, most evident on ventro-flexion. The condition may occur concurrently with immune-mediated polyarthritis (IMPA) manifesting as joint pain and effusions, typically of small joints, i.e., carpi/tarsi. Vasculitis has also been described leading to pleural effusion and spontaneous haemorrhage, including associated with the spinal cord. Both acute and chronic forms are described, and it is not unusual for clinical signs to wax/wane or seemingly improve with other treatment (e.g. use of non-steroidal anti-inflammatory drugs).

Figure 1: A dog shows a low 'head carriage' suggestive of cervical pain.
Aetiology: An excessive immune-response targeting the meninges results in suppurative inflammation, necrotising arteritis, fibrosis and haemorrhage. In chronic cases, vessel stenosis is seen. Neutrophil infiltration into the cerebrospinal fluid (CSF) results, facilitated by chemotactic factors and upregulation of integrins and metalloproteinases that disrupt the blood-cord-barrier. Although it is deemed an immune-mediated aetiology, no specific trigger factors have been found, other than breed predisposition.
Diagnosis: Haematology and serum biochemistry may reveal a systemic inflammatory response including a neutrophilia, hyperglobulinaemia and hypoalbuminaemia. Acute phase proteins are often elevated including C-reactive protein (CRP) and serum immunoglobulin A. Although non-specific, CRP has also been used as a marker for remission in cases of SRMA. Imaging should be performed to investigate other causes of cervical pain (see Table 1). In patients in which SRMA is highly suspected, radiographs may be sufficient to exclude differentials such as atlanto-axial instability, cervical trauma and discospondylitis prior to CSF sampling. Alternatively, advanced imaging such as CT or MRI may be used. These may often be normal or show meningeal contrast enhancement in cases of SRMA, however would also facilitate exclusion of other differential diagnoses including but not limited to discospondylitis, intervertebral disc extrusion/protrusion, neoplasia, malformation or other meningoencephalomyelitis of unknown aetiology.
CSF sampling is the most sensitive and specific test. It should be obtained from the site nearest that of clinical signs (i.e., cerebellomedullary cistern in dogs with neck pain) to help increase the likelihood of detecting abnormalities, however often both cisternal and lumbar CSF samples are advised. CSF typically shows a neutrophilic pleocytosis with marked elevations in cell count and total protein. The neutrophils appear non-degenerate, in contrast to bacterial meningitis, which is typically associated with degenerate neutrophils. Although an important differential for neutrophilic pleocytosis, the latter is much less common in dogs and often accompanied by signs of more severe systemic/neurological compromise.
Treatment and prognosis: Treatment consists of immunosuppressive doses of corticosteroids, typically tapering over an approximate six-month period. A proposed protocol is described by Lowrie et al, 2009. In this study, all dogs responded to prednisolone monotherapy, however a 20 per cent relapse rate was reported. Although recurrence is possible, either at lower doses of steroids or following cessation of treatment, these may be managed by returning to a higher dose protocol and attempting to taper once again. A second immunomodulatory agent can also be considered such as azathioprine, leflunomide or cytosine arabinoside.
Prognosis is typically considered good to excellent, with up to 80 per cent of cases going into long-term remission. However, recurrence of the disease, particularly with rapid tapering of corticosteroids, is possible.

Table 1: Differential diagnoses for possible causes of cervical pain in dogs using the VITAMIN-D acronym.
Note: metabolic causes are not included.
SRMA (steroid-responsive meningitis-arteritis); IMPA (immune-mediated polyarthritis); MUA (meningoencephalitis of unknown aetiology).
Meningoencephalitis of unknown aetiology/origin (MUA/MUO)
The term MUA or MUO encompasses several immune-mediated inflammatory CNS disorders including granulomatous meningoencephalitis (GME), necrotising meningoencephalitis (NME) and necrotising leucoencephalitis (NLE). As it is not possible to distinguish between these distinct entities ante-mortem, the MUA umbrella term is used. Importantly, MUA is the most common immune-mediated inflammatory condition of the CNS, accounting for 47.5 per cent in one study, followed by SRMA at 30.7 per cent.
Signalment: Typically young to middle-aged small breed dogs are predisposed to MUA. Specifically, middle-aged toy and terrier breeds appear to be predisposed to GME, and Yorkshire terriers to NLE, while NME (also once termed ‘pug encephalitis’) tends to affect younger toy and small breed dogs including Pugs, Yorkshire Terriers, Maltese, Chihuahuas, Pekinese, Papillons, Shih Tzus, Coton de Tulears and Brussels Griffons. However, all breeds may be affected with a more recent study of 111 dogs documenting 25 per cent of those affected were large breeds (> 15 kg). One study found that dogs with the necrotising forms are significantly more likely to present at a younger age (predominantly < four years old) in comparison to GME at four to eight years. Although studies are lacking, given their frequent presentation (in part likely a result of a marked increase in popularity), the author also suspects French Bulldogs are predisposed to this condition.
Presentation: Signs are typically acute in onset and rapidly progressive. Clinical presentation is dependent on localisation of the CNS lesion/lesions and so is highly variable but may include abnormal mentation, cranial nerve deficits, paresis, ataxia, vestibular dysfunction and seizures. In severe cases, cluster seizures, status epilepticus, stupor or coma may result. In the case of GME, three histological distribution patterns have been described; optic, focal or multi-focal/disseminated. In dogs with optic GME, the only clinical sign may be acute onset blindness (uni- or bilateral). In one study, eight percent of dogs diagnosed with GME presented with signs suggestive of a myelopathy only, and so MUA should still be considered as a differential diagnosis in spinal cord dysfunction.
Aetiology: Although no underlying cause has been identified, a multifactorial combination of familial predisposition, infectious agents or immunopathological mechanisms have been proposed. Given the response to immunosuppressive therapy, an immune-mediated aetiology is suspected.
Diagnosis: Diagnosis is made based on a combination of signalment, clinical examination, MRI and CSF analysis. MUA is considered ultimately a fatal condition without treatment and so should be considered as an important differential diagnosis for any young-middle aged small breed dog with acute and progressive central neurological signs. MRI often shows multi-focal asymmetrical poorly demarcated intra-axial lesions that may affect the cerebrum, brainstem and/or cerebellum, with varying degrees of contrast enhancement (see Figure 2). These lesions may produce mass effect or in severe cases herniation of brain tissue due to raised intra-cranial pressure. In cases with clinical or radiological concerns of raised ICP, CSF collection is contraindicated. CSF typically shows a marked elevation in total nucleated cell count (TNCC; reference < five white blood cells /μL) and total protein (TP; reference <0.25 mg/dL), with a mononuclear pleocytosis. In one study, four inclusion criteria for diagnosis were described: dogs older than 6 months of age; multiple, single or diffuse intra-axial hyperintensities on T2-weighted (T2W) MR images; pleocytosis on CSF analysis with >50 per cent of monocytes/lymphocytes; and lastly, exclusion of infectious diseases.
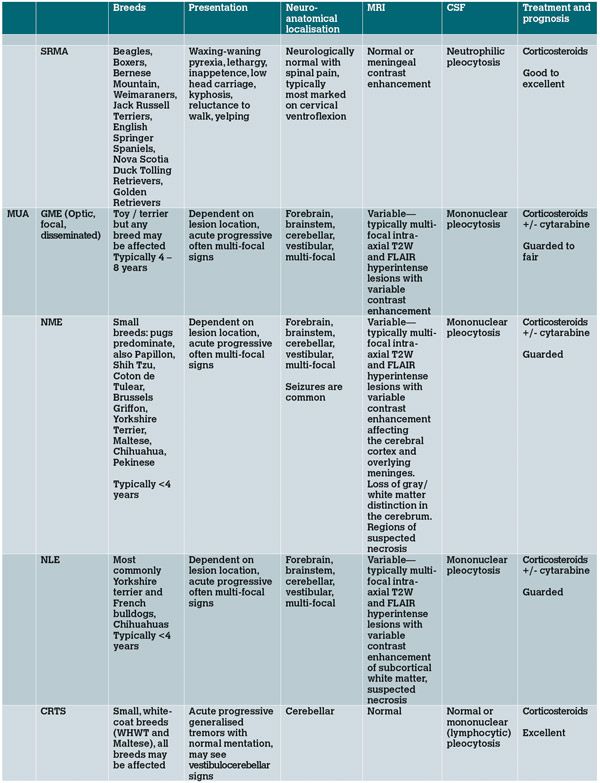
Table 2: Comparison of most common non-infectious inflammatory CNS conditions.
Although brain biopsy procedures have been described in the literature, these are rarely performed due to the associated morbidity and cost.
Treatment and prognosis: The mainstay of treatment is immuno-suppressive doses of corticosteroids, typically administered as intravenous dexamethasone for two to three days prior to transitioning to oral prednisolone. There are many studies reviewing the use of adjunct immune-suppressive therapy with multiple studies supporting the clinical efficacy of cytosine arabinoside (cytarabine). Treatment with a second immunosuppressive agent also allows more rapid tapering of prednisolone.
Additional treatment in the emergency setting may be required. Important considerations include seizure management, respiratory compromise and raised intracranial pressure. The latter may be suspected if there is reduced or progressively deteriorating mental status, miosis, anisocoria or mydriasis. It is also possible to see progressive bradycardia, hypertension and an abnormal breathing pattern (also termed Cushing’s response/triad) that is indicative of severe or even terminal brain stem dysfunction. If an elevation in intracranial pressure is suspected, treatment should be initiated with either Mannitol (0.25-1g/kg of 10 per cent solution over 10-15 minutes) or seven per cent hypertonic saline (4ml/kg in dogs, 2ml/kg in cats IV over 15 minutes).
This should be followed with isotonic fluids to restore fluid balance and electrolytes and to prevent hyperosmolarity. The head should be elevated to facilitate venous drainage and blood sampling using the jugular vein should be avoided (venous occlusion will elevate ICP).
Seizures must be promptly managed with benzodiazepines, levetiracetam and/or phenobarbitone as appropriate. Specific emergency textbooks should be consulted for further information on seizure management.
Prognosis is highly variable, although generally considered guarded, and may depend on severity of presentation. One study documented that 15 per cent of dogs with GME died prior to initiation of treatment and, in a second, 56 per cent of dogs died or were euthanised despite treatment, 33 per cent of these within three days of diagnosis. Another study reported similar results with 25 per cent of dogs dying or being euthanised within seven days of diagnosis. Despite this, good outcomes are possible with many dogs returning to normal. However, long-term treatment is typically required and clinical relapse of the disease is possible.
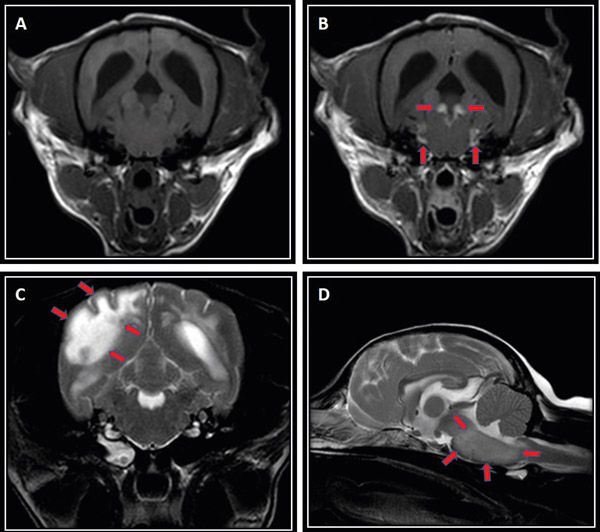
Figure 2: MRI sequences of dogs diagnosed with MUA; T1-weighted transverse image at the level of the pons pre-(A) and post-gadolinium (B) contrast administration. Note the bilateral marked contrast enhancement and thickening of the meninges at this level (red arrows). In another dog with suspected NLE (C), marked asymmetrical T2-weighted hyperintensity is seen on transverse sequence, most predominantly affecting the occipital lobe with loss of white/grey matter distinction (red arrows). The brainstem may also be affected as seen in another dog (D) with diffuse ill-defined T2-weighted hyperintensity and generalised swelling seen on sagittal sequence (red arrows).
Corticosteroid-responsive tremor syndrome
CRTS, also know as idiopathic generalised tremor syndrome (IGTS), ‘little white shaker disease’ or idiopathic cerebellitis, manifests as acute onset generalised body tremors with otherwise appropriate mentation.
Signalment: Young, small breed dogs are typically affected including the West Highland White Terrier and Maltese, usually between one to five years of age.
Presentation: Dogs typically present with acute onset rapid fine tremors affecting the head, trunk and limbs that can progress over the first one to three days. The tremors tend to worsen with stress and excitement, reduce with relaxation and resolve with sleep. The tremors can result in hyperthermia. Occasionally, additional clinical signs such as absent menace response, head tilt, nystagmus or opsoclonus have been reported.
Diagnosis: A major differential diagnosis of acute onset generalised tremors is toxin exposure, e.g., mycotoxin ingestion, pyrethrin/organophosphate, lead, metaldehyde. It is important to ascertain from the clinical history if exposure to one of these is possible (such as onset after a walk, ingestion of mouldy food) and specific treatment administered if so. Should dogs be treated for suspected toxin exposure and not show improvement within 48-72 hours, this may make other causes such as CRTS more likely. There are many causes of tremors in dogs, including physiological (e.g., stress-induced, hypothermia), hypocalcaemia or hypoglycaemia. More specific recognised neurological disorders include orthostatic tremors, idiopathic head tremor syndrome (‘head-bobbing’), hypomyelination disorders, storage diseases or degenerative CNS disease. Other abnormal movement disorders such as paroxysmal dyskinesia or seizure activity may also be considered. Diagnosis involves exclusion of these other differentials, including MRI to exclude any structural pathology and CSF analysis. MRI is typically normal, and CSF may be normal or can show a mild to moderate lymphocytic pleocytosis.
Treatment and prognosis: Benzodiazepines such as midazolam, or other sedatives may be used for emergency management of the tremors. Specific treatment consists of a tapering course of immuno-suppressive corticosteroids. Although there is no set protocol, as a general guide we tend to start with 2mg/kg/day and taper the dose by 20-25 per cent every three to four weeks thereafter. Prognosis is considered good to excellent with most dogs returning to normal within days of initiating treatment, however, recurrence of clinical signs is possible.
Other inflammatory conditions:
Several rarer non-infectious inflammatory conditions of the CNS have been described in dogs.
Idiopathic hypertrophic pachymeningitis has been well described in humans and more recently in dogs. It results in chronic inflammation and thickening of the dura mater leading to a range of central neurological signs. Dogs affected according to the relevant report included middle-aged Greyhounds and Labrador Retrievers, typically presenting with abnormal mental status and varying cranial nerve deficits. MRI showed diffuse pachymeningeal thickening and a lymphocytic pleocytosis on CSF in the majority of cases. There is limited information regarding prognosis however it would seem more guarded with fewer dogs responding to treatment compared to other inflammatory conditions.
Eosinophilic meningoencephalitis of unknown origin has also been described in dogs, with Rottweilers and Golden Retrievers over-represented. Dogs are typically young to middle-aged larger breed dogs, presenting with varying CNS signs including altered mentation, cranial nerve deficits, paresis and ataxia. MRI shows multi-focal/diffuse regions of meningitis/encephalitis as well as cortical atrophy. As the name suggests, CSF documents an eosinophilic pleocytosis. Elimination of infectious causes such as Neospora caninum and Toxoplasma gondii is important, either by serology or PCR on CSF. Again, this condition is thought to be immune-mediated, however the underlying pathogenesis remains unknown. Treatment with immuno-suppressive corticosteroids +/- cytosine arabinoside has been described with good response. Given its rare prevalence, literature is limited on best treatment and prognosis.
A meningoencephalitis of young Greyhounds has also been described, originating in Ireland, and frequently affecting multiple litter mates. The clinical signs are seemingly more chronic in onset in comparison to other CNS diseases (from five days to 12 months) and highly variable with lethargy, weight loss, paresis, ataxia, circling, altered vision and cranial nerve deficits reported. MRI findings show multi-focal bilateral lesions predominantly affecting the olfactory, frontal, and temporal cortical gray matter, and caudate nuclei. CSF typically shows a mild to moderate mononuclear pleocytosis in the absence of identified infectious organisms. Corticosteroid treatment was provided in some patients but the prognosis appears poor with the condition ultimately proving fatal.
Although not discussed in this article, various other inflammatory conditions can affect the peripheral nervous system including polyneuropathies (such as acute polyradiculoneuritis) and polymyopathies (such as idiopathic inflammatory polymyositis of Hungarian Vizslas, masticatory myositis).
Conclusion
Immune-mediated inflammatory conditions affecting the CNS are a common neurological presentation. Both signalment and clinical history can indicate likely differentials and appropriate diagnostic tests. Prognosis is highly variable between conditions and emergency treatment such as management of status epilepticus and elevated intracranial pressure may be required. Although cases often result in referral to specialist institutions, knowledge of these conditions can result in appropriate care and treatment. In severe cases where the extent of neurological involvement may be life-threatening, prompt recognition and treatment may improve outcome for patients.
References available on request.
Acknowledgments
The author would like to thank Dr Abbe Crawford for review of this paper.
1. What is typically NOT a common feature of steroid-responsive-meningitis-arteritis?
A. Pain on cervical ventro-flexion or diffuse spinal pain
B. Systemic neutrophilia
C. Neurological deficits
D. Elevated acute phase proteins such as C-reactive protein
2. Which type of pleocytosis is typically seen in the CSF of SRMA cases?
A. Mononuclear
B. Neutrophilic
C. Lymphocytic
D. Eosinophilic
3. What is not a classified form of GME?
A. Spinal
B. Optic
C. Disseminated
D. Focal
4. Which adjunctive immuno-therapy has been most commonly used in cases of MUA?
A. Azathioprine
B. Cytarabine (cytosine arabinoside)
C. Ciclosporin
D. Leflunomide
5. What signalment is corticosteroid-responsive tremor syndrome most commonly associated with?
A. Dogs < six months old
B. Large breed dogs
C. Pugs and Yorkshire terriers
D. West Highland White Terriers and Maltese
Answers: 1C; 2B; 3A; 4B; 5D.














