Small animal - December 2019
Local and regional anaesthetic techniques in small animals – part 2
Lisa McAuliffe VN BSc BVSc CertVOphthal MSc VAA MRCVS presents part two of a two-part series that focuses on local and regional anaesthetic techniques
There is now a wealth of good quality evidence for the analgesic, safety, MAC sparing and side-effect limiting effects of a variety of local nerve blocks for orthopaedic and soft tissue models.
Many of us don’t venture to learn or perform them due to time, invasiveness, cost and fear of adverse events but by using local anaesthetics we provide an inexpensive means of pain relief and a rapid return to normalcy without the opioid side effects for our patients, something both equine and farm practitioners have known for years!
Epidural, local blocks or regional blockades can be administered under heavy conscious sedation or general anaesthesia. The site should be prepared aseptically. Anatomic landmarks can be used to place several blocks ‘blindly’, however, advances are being made with the use of ultrasonography and electrostimulation and there are fantastic online resources (such www.zeropainphilosophy.com, which has very useful videos and information to aid the practitioner).
Positioning & Equipment
Patient positioning is extremely important to nerve location as this can easily alter as nerves are flexible structures. In some instances, patient positioning may also affect the drug distribution, so correct placement of the patient prior to location and injection should be considered. Using described standardised positioning and techniques helps minimise complications.
Most of the equipment required for these techniques are readily available from most veterinary suppliers but some more specialised items can be ordered from medical equipment companies.
There are a wide variety of needles available for use, and these are generally selected based on their physical characteristics. The length of the needle selected depends on the anticipated target nerve. Smaller gauge needles are often used for infiltration anaesthesia or superficial blocks, and larger gauge needles are used in deeper tissue blocks e.g epidurals, brachial plexus blocks.
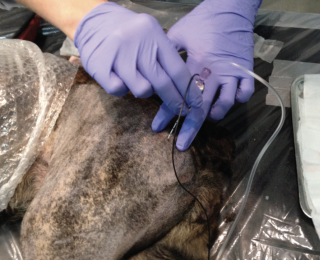
Nerve blocks can be performed blindly using palpation and landmarks, via ultrasound or using a neurostimulation technique. Electrolocation or neurostimulation of nerves and nerve roots can be performed using a peripheral nerve stimulator, which uses a microcurrent directed down a sheathed needle (Figure 1).
When the needle tip is proximal to the intended target nerve, a small motor response is seen. Ultrasound guided electrostimulation is also useful and allows correct needle placement without damage to blood vessels or the nerve itself.
Thoracic Blocks
The infusion of local anaesthetics into the interpleural space and the selective intercostal nerve blocks are easy to incorporate into an analgesic plan for any patient undergoing thoracic surgery. With either of these techniques, it is important to dilute the local anaesthetic drugs required and provide appropriate dosages.
Intercostal nerve block
This technique is easy to perform as the nerves can be seen and palpated during thoracic surgery. The nerves have two purposes; some nerve fibres provide the intercostal muscles with their motor function, and others provide sensory innervation via lateral branches to the skin lying over the lateral and ventral chest wall.
The site of puncture should be made as proximal as possible on the lateral aspect of the rib cranial to the incision. The needle can be walked off the back of the rib into the intercostal space but not advanced enough to penetrate beyond the depth of the intercostal muscles into the pleural space.
Aspiration should be performed to check for blood or air. Following calculation of the maximum dose for the patient, an appropriate volume of local anaesthetic is slowly injected.
It is generally recommended that 2-3 nerves blocked both cranial and caudally to the wound will provide good analgesia.
Interpleural regional anaesthesia
As the pleura has a large surface area, there is both the potential for rapid absorption and elevated plasma levels of local anaesthetic to result from this technique which consequently may lead to systemic toxicity. To avoid repeated injections, it is possible to place an indwelling catheter to deliver appropriate dosages to this site.
Thoracic Limb blocks
Both the cervical paravertebral and the brachial plexus blocks have been demonstrated to provide anaesthesia and analgesia to the proximal thoracic limb. The cervical paravertebral block is an – advanced – level technique that has a potentially high level of complications (Lemke et al, 2008) and will not be described here.
Brachial plexus blocks
The goal is to block the plexus supplying the thoracic limb and three approaches have been described. The author uses an ultrasound-electrolocation guided approach where the patient is placed in dorsal recumbency. The transducer is placed over the axillary region in a fossa that exists between the manubrium and the supraglenoid tubercle of the scapula (Figure 2) and is orientated in a para-saggital plane until the axillary vessels are seen (‘double‐bubble’ sign) and the roots of the brachial plexus can be visualized.
The root of C8 should be identified as located immediately dorsal to the axillary artery, and the stimulating needle inserted dorsal to the cranial edge of the pectoralis muscle and lateral to the jugular vein. The needle is advanced in a cranial-to‐caudal direction, keeping the tip in the field of ultrasound view at all times. Contractions of the triceps brachii muscle, resulting in elbow extension should be observed. Care must be taken to avoid the axillary vessels.
Following appropriate dosage calculations for the patient, the recommended volume of local anaesthetic to be injected for a brachial plexus block is 0.15–0.2mL/kg (Campoy et al, 2008).
RUMM Block
Useful when performing surgery on the distal areas of the forelimb, this blocks the radial, ulnar, median and musculocutanous nerves and has two injection sites. On the lateral aspect the limb, it is possible to palpate the radial nerve as it traverses the mid to distal third of the humerus (Figure 3). The second site is via a medial approach to the limb where it is possible to palpate the mid shaft of the humerus and move the biceps brachii cranially to block the ulnar, median and musculocutaneous nerves. The recommended volume to be injected for the radial nerve (lateral site) is 0.1 mL/kg and for the musculocutaneous, median, and ulnar nerves 0.15 mL/kg.
Pelvic limb blocks
Femoral nerve
There are various suggested approaches to blocking the nerves of the pelvic limb. The medial femoral triangle approach to the femoral nerve and the lateral approach (ischiatic tuberosity–greater trochanter line approach) for the sciatic nerve are described here as they have relatively low complication rates and have an intermediate level of difficulty associated with them.
To avoid femoral artery and vein puncture, the use of electrostimulation is advised. The patient is positioned in lateral recumbency with the limb to be blocked positioned uppermost, abducted 90° and extended caudally (Figure 4).
With the transducer placed over the femoral triangle, in a cranio‐caudal direction, a short‐axis view of the femoral vessels and the nerve should be obtained. The recommended volume to be injected is 0.1 mL/kg (Costa-Farre, 2011). A combination of bupivacaine 0.5% and dexmedetomidine (0.5–2 µg/mL of injectate solution can be used to provide surgical anaesthesia.
Both the femoral and sciatic nerves must be blocked for almost any stifle procedure.
Sciatic nerve block
The sciatic nerve block if used alone, is sufficient to perform surgery of the foot and hock (Figure 5).
With the patient positioned in lateral recumbency, it is important to first locate the greater trochanter and ischiatic tuberosity. The puncture site is located at the point between the cranial and the middle thirds of a line that is drawn between these two landmarks. Once close to the sciatic nerve, dorsiflexion or plantar extension of the foot will be elicited. The recommended volume to be injected is 0.05–0.1mL/kg.
Epidurals
Epidural analgesia involves the deposition of substances above the dura or covering the meningeal layers and is most commonly used for hindlimb or abdominal analgesia, but with drug dilution and an increase in volume, it can be used for spinal or thoracic surgeries as well. For repetitive boluses or continuous small volume infusions, epidural catheters and small pumps can be utilised.
They should not be used in patients with elevated intracranial pressure, those with clotting disorders or those with uncorrected hypovolaemia and hypotension. Epidural anaesthesia should be avoided in patients with skin infections or evidence of neoplasia at the site of injection.
The best entry site for administration is the lumbosacral space (L7-S1) as it is a relatively wide intervertebral space at this location. A sacrococcygeal approach to the epidural space has been described in cats, which minimises the risk of dural puncture and assists in facilitating urethral catheterisation in blocked cats (O’Hearne, 2011).
To perform an epidural injection, the animal may be placed in either sternal or lateral recumbency, and the puncture site is located between the dorsal spinous processes of L7 and S1 (Figure 6).
The needle is advanced through the supraspinous and interspinous ligaments and resistance will be observed. Several methods have been developed for identifying the epidural space, including the use of a ‘hanging drop,’ ‘loss of resistance,’ and, more recently, electrostimulation.
Pressure within the epidural space has been reported to be anywhere from –6 to +15mmHg in dogs. If a drop of saline or local anaesthetic solution is placed in the hub of a Tuohy or spinal needle, as the needle penetrates the epidural space it will usually be aspirated into the space.
Resistance to injection of air or fluid is felt while the needle is advanced through the intervertebral ligaments. If pressure is being applied to the plunger of a ‘loss of resistance’ (LOR) syringe, a sudden loss of resistance to injection will be appreciated when the needle punctures the ligamentum flavum and enters the epidural space. A false‐positive result may ensue if the needle is located within the intervertebral fat. This technique is not commonly used.
Bupivacaine and lidocaine are frequently used in the epidural space, with bupivacaine giving a longer duration of action. Opioids such as morphine (preservative free) can also be used in combination. The volumes used control the cranial spread of the drugs. Care must be taken when calculating drug volumes.
The body condition score of the patient should also be considered as an obese animal may have more epidural fat than lean animals, reducing the available space for the drugs within the epidural space so the volume may have greater cranial spread than expected.
Urinary retention is probably the most commonly reported side effect of epidurals and particularly epidural opioids. Other side effects such as pruritis have also been reported.
Intraarticular blocks
Intraarticular blocks can be used before or after joint surgery, eg, for arthroscopy. A single use of local anaesthesia is unlikely to have a significant detrimental effect on cartilage however continued use may cause damage. The selection of local anaesthetic has also been shown to be important as ropivacaine has appeared to cause less of an effect on cartilage than bupivacaine (Sung, 2014).
- Lemke KA, Creighton CM. (2008) Paravertebral blockade of the brachial plexus in dogs. Veterinary Clinics of North America Small Animal Practice, 38(6): 1231–1241.
- Campoy L, Martin‐Flores M, Looney AL. (2008) Distribution of a lidocaine–methylene blue solution staining in brachial plexus, lumbar plexus and sciatic nerve blocks in the dog. Veterinary Anaesthesia and Analgesia, 35(4): 348-354.
- Costa‐Farre C, Blanch XS, Cruz JI. (2011) Ultrasound guidance for the performance of sciatic and saphenous nerve blocks in dogs. Veterinary Journal, 187(2): 221-224.
- O’Hearn AK, Wright BD. (2011) Coccygeal epidural with local anaesthetic for catheterization and pain management in the treatment of feline urethral obstruction. Journal of Veterinary Emergency & Critical Care, 21(1): 50-52.
- Sung, Chang-Meen. (2014) Cytotoxic Effects of Ropivacaine, Bupivacaine, and Lidocaine on Rotator Cuff Tenofibroblasts. The American Journal of Sports Medicine, 42(12), pp.2,888-2,896.
1. Which block can be selected for hock surgery?
a. Interpleural
B. Medial femoral triangle
C. Mental foramen
D. Sciatic nerve block
2. The radial nerve can be easily palpated on the
a. Lateral aspect of the humerus
B. Medial aspect of the humerus
C. Medial aspect of the biceps brachii
D. Lateral aspect of the calcaneous
3. Which nerve root is dorsal to the axillary artery?
a. C7
B. C8
C. C4
D. C5
4. Epidurals should not be used when:
a. Patient has hypotension
B. Patient has a clotting disorder
C. Patient has hypovolaemia
D. All of the above
5. Which local anaesthetic is potentially less damaging to cartilage?
a. Lidocaine
B. Ropivacaine
C. Bupivacaine
D. proparacaine
Answers: 1:D; 2:A; 3:B; 4:D; 5:B