Large animal - September 2019
Nursing care of the pregnant mare with laminitis
Shannon Brereton, BSc in Veterinary Nursing, Dundalk Institute of Technology, outlines the management and care of a pregnant mare with laminitis
Introduction
Laminitis is defined as inflammation of the lamellae, resulting in failure of the attachment between the distal phalanx and the inner hoof wall (Pollitt, 2004). Without the distal phalanx securely attached to the inner hoof wall, the weight of the horse forces the bone down into the hoof capsule (Figure 1). This action causes damage to the arteries and veins, crushing the corium of the sole and coronet, causing severe pain and a characteristic lameness (Pollitt, 2004).
Laminitis is classified by its duration and morphological changes that occur in the distal phalanx (Parks 2009). The initial phase, known as the developmental phase, occurs between the initial insult and the onset of clinical symptoms. This is then followed by the acute phase, which lasts up to 72 hours after the onset of clinical symptoms (McDonnell 2017). Chronic laminitis begins with the displacement of the distal phalanx, where long-term management is necessary (Parks 2009). Therefore, it is important to understand the clinical signs of this disease in order to treat it early and optimise recovery.
Excellent nursing care is very important for the treatment of laminitis in the pregnant mare. It promotes recovery and improves quality of life by providing optimal care and pain management. The nurse's role can also include dealing with clients by assisting with queries, as well as clarifying the condition, causes, available diagnostic tests, nursing and treatment plans, further treatment options and possible outcomes (McDonnell, 2017).
Pain scoring
As veterinary nurses, it is our responsibility to make our patients as comfortable as possible. We need to be able to evaluate behavioural changes that are associated with pain in horses. Observing the horse’s posture, facial expressions (pain face) and attitude can detect signs of pain. The common presenting signs of pain associated with laminitis include: reluctance to move or increased time lying down, and an attempt by the horse to carry all its weight on its heels, resulting in the characteristic leaning back stance and heel-first footfall when walking (Coumbe, 2001).
The ‘pain face’ is a validated scoring system used to quantify equine pain. It is best to evaluate facial expressions when the horse is undisturbed. However, an animal experiencing severe pain will continuously express a ‘pain face’. The areas of interest when looking at facial expressions for pain are the moveable parts: ears, eyes, lower facial muscles, nostrils and muzzle (Gleerup, 2018). The ears can take several positions when a horse is experiencing pain. They will respond less to their surroundings while positioning lower and further back than usual. Muscles around the eyes will appear tense and give an angular shape to the eyebrow.
Tension around the eyes, due to pain, will result in a tense stare with less focus on the surrounding environment. Nostrils can appear dilated but may only be visible during inspiration. The lower facial muscles will also appear tense with the lips compressing firmly together. An overall evaluation of the equine pain face will result in a tense/strained appearance (Figure 2). Equine facial expressions are a useful communication tool when working with horses and can be used for detecting low-to moderate-degree pain, especially within the early stages of laminitis (Gleerup, 2018).
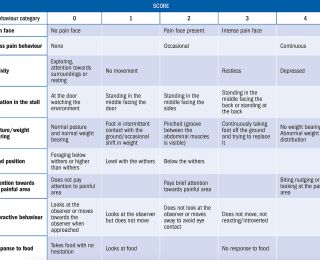
A pain scoring chart is a useful tool which is used to evaluate if the pain management method put in place is successful (Table 1). This comprehensive scoring chart is combined with the evaluation of the pain face and more traditionally used methods, ie. interaction, posture or aggression/behaviour. Evaluation of pain through the equine pain scale can be performed within two minutes, which proves to be practical in an equine hospital. Using this scale, the mare should be scored twice daily, morning and evening, to identify any changes in pain, which can contribute to the nursing plan and tailor the analgesic protocol.
Medical therapy
The failure to adequately control pain is a common reason for which horses afflicted by laminitis are ultimately subjected to euthanasia (Bamford 2019). Non-steroidal anti-inflammatory drugs (NSAIDs) such as flunixin meglumine (1.1mg/kg PO or intravenous [IV] SID to TID) and phenylbutazone (2-6mg/kg PO SID to BID), at low dosages, are commonly used as a form of analgesia, and to treat the inflammatory responses induced by laminitis. For chronic stage laminitis cyclooxygenase type 2 (COX-2) inhibitor class NSAIDs, such as firocoxib, provide safe and effective pain relief. Non-selective COX inhibitors may be best in the developmental and acute stages of laminitis, as the vascular function is still present (Orsini, Wrigley and Riley, 2010). A vasodilator such as acepromazine (0.002-0.0066mg/kg PO or IV or intramuscular [IM]), is beneficial to counter vascular dysfunction in the digit (Parks, 2009). Acepromazine increases digital and laminar blood flow in normal horses. The tranquillising effects of acepromazine may encourage the horse to lay down, which can be beneficial. More recently, interest in using other analgesic agents such as lidocaine and ketamine – given as an intravenous infusion – or narcotics either as a continuous rate infusion or epidural, has developed (Parks, 2009).
Horses that have developed laminitis associated with insulin resistance (IR) such as equine metabolic disease may benefit from early intervention to increase insulin sensitivity (O’Grady, 2013). Physiological stress in the form of pain can result in a decrease of insulin by increasing circulating catecholamines which inhibit insulin production (Gordon et al, 2007). Therefore, introducing medical therapy early can alleviate the stress caused by pain. Broodmares are at particular risk of endocrinopathic laminitis (EL) due to their decrease in insulin sensitivity associated with pregnancy (Galantino-Homer and Engiles, 2012). EL can also be managed through blood testing for endocrinopathic changes, thyroid hormone supplementation and normalisation of weight and serum insulin through diet. Registered veterinary nurses (RVNs) should consult with an equine nutritionist when caring for a laminitic pregnant mare in order to meet the nutritional needs of the mare. Ideally, weight and insulin normalisation should be established prior to pregnancy, as pregnancy-associated IR can push the threshold for EL (Galantino-Homer and Engiles 2012).
NSAIDs should not be the sole agents used for pain management during pregnancy. Chronic pain and increased NSAID intake can result in the birth of a very weak and underdeveloped foal (Dowling, 2019). Often these drugs fail to achieve adequate pain relief and have the potential for adverse effects with long-term administration (Bamford, 2019). Care must be taken with NSAID use to monitor for gastric ulceration and ensure the horse is drinking well (Orsini, Wrigley and Riley, 2010). Clinical signs of gastric ulceration include bruxism (grinding of teeth), abdominal pain after eating and weight loss (Bassert, Beal and Samples, 2018). Anti-ulcer medications can be used to prevent and treat gastric ulceration, such as omeprazole (GastroGard). Right dorsal colitis and necrotising colitis can result from the overuse or misuse of phenylbutazone (El-Ashker et al, 2012). Exposure of the colonic mucosa to anti-inflammatory drugs can result in erosions and ulceration due to the high production of free radicals. The risk of gastric ulceration, renal failure and colitis due to phenylbutazone is exuberated in a dehydrated or hypovolaemic patient. In this case, fluid therapy may be administered at 30-50ml/kg/day (El-Ashker et al. 2012). Phenylbutazone should only be given to minimal effective dose with no more than four grams per day administered to a full-size horse (Bassert, Beal and Samples, 2018).
Hydration status, plasma protein levels and renal values should be monitored in horses receiving prolonged treatment with NSAIDs. These can be monitored by daily evaluation of urine specific gravity (USG) using a refractometer and/or collecting a serum biochemistry blood sample. USG should remain between 1.025-1.060, in a hydrated horse. A biochemistry blood panel will indicate renal failure and dehydration through elevated levels of albumin, blood urea nitrogen (BUN), creatinine, total protein (TP) and sodium. By collecting a haematology blood sample, a packed cell volume (PCV) and TP concentration can also be evaluated. The plasma protein concentration is visualised on a refractometer where values should remain between 5.7-7.2g/dL. PCV values should remain between 27-43%: elevated PCV and TP levels are indicative of haemoconcentration or dehydration.
Hoof care and housing
Pregnant mares are often unshod. However, in the instance of a pregnant mare with laminitis supportive shoeing/padding may aid in pain control and comfort. Therapeutic shoes/pads have proved beneficial in the laminitic horse, as they reduce hoof overloading and increase comfort (Bamford, 2019). These supportive therapeutic shoes work by moving the centre of pressure and adjusting the distribution of pressure from the hoof wall to the sole. This is achieved by stabilising the distal phalanx, as this reduces stress on the affected lamellae. There are a variety of methods out there which are used to achieve this effect. The most commonly and effectively used methods include the application of a styrofoam board and commercial boots (Parks 2009).
Various methods can be tried to find the horse’s preference. Observation of the mare's response, using the pain scoring chart, will illustrate effective pain-free and supportive care. Regular hoof trimming is also essential to increase blood flow within the digital circulation (Wrigley, 2011). This can be performed by a specialised farrier every six to eight weeks, depending on hoof growth. The pads/shoes should be checked and cleaned or changed once or twice daily. Daily foot care is important but can be difficult in the laminitic mare, as she may be reluctant to lift her feet. Optimal pain relief, deep bedding and solar support will facilitate daily hoof care. If the mare is in extreme pain and reluctant to lift her feet, sedation such as detomidine hydrochloride (0.01-0.02mg/kg IV or IM or PO) can be administered (O’ Grady, 2013). Abaxial nerve blocks are also beneficial to facilitate standing for digital radiography etc. in the laminitic horse (Gardner, 2011). During daily foot-care procedures, it is important to assess the intensity of digital pulses and the temperature of the feet. Elevated digital pulses and temperature indicate foot pain and inflammation.
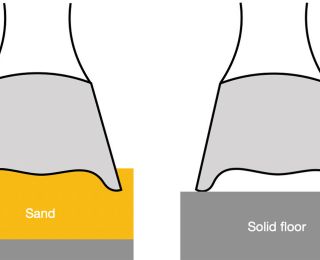
The horse’s environment should also be considered. Additional factors are required to meet the pregnant mare's needs. As nurses, it is our job to ensure the mare is in optimal comfort throughout her pregnancy. Housing should be warm, safe, dry, well ventilated, draught free, quiet, clean, comfortable and spacious. The stable should ideally be 14ftx14-16ft. This ensures adequate room for moving around, lying down to rest and foaling. A large stable also reduces the risk of the mare becoming cast. The bedding should be deep enough to provide solar support and aid mobility. Conformable substrates such as deep sawdust, shavings or peat are suitable (Wrigley 2011). Arena surfaces or stalls with beach sand are also extremely beneficial. The properties of the sand allow the toe of the hoof to sink in and elevate the heel, this distributes bodyweight across the foot and provides comfort to the horse (Figure 3).
The bedding should always be kept dry and clean from manure and urine, as the horse may spend most of its time standing or resting in one spot. Damp or dirty bedding can increase the risk of foot abscesses in the chronic stages of laminitis (Wrigley, 2011).
Rehabilitation and cryotherapy
In the acute and chronic stages, movement/exercise and stress on the lamellae can result in increased damage and should be avoided. However, movement and exercise are very important components to the physical and physiological wellbeing of the horse and can be beneficial for the recovery from laminitis (Wrigley, 2011). Rehabilitation should be done gradually. The patient may be stiff and experience pain when walking, especially on hard surfaces. Standing around in a stable will not improve recovery or quality of life and can often lead to stiffness and soreness within the muscles of their shoulders, back and hind-quarters (Wrigley 2011).
In the developmental and acute stages, simple exercises can be performed to stretch the limbs to release tension and prevent tension build-up in the deep digital flexor tendon. These can be achieved by gently extending the forelimb cranially and repeating on the opposite side. This exercise stretches the myofascial tissues along the palmar/caudal aspect of the forelimb all the way to the trunk (Wrigley, 2011). If the mare is too sore to perform these exercises different types of physiotherapy such as effleurage, petrissage, and friction can be carried out. These types of massage help warm the underlying muscle; improve circulation; break down adhesions; and promote drainage of lymph channels. This range of physiotherapy can be performed daily to increase mobility and comfort. Care must be taken to ensure the horse's comfort and then sessions can be increased with improvement.
Digital hypothermia (cryotherapy) is a therapeutic intervention that has be shown to provide analgesia and reduce the severity of sepsis-related laminitis (Bamford 2019). To successfully achieve effective pain relief, the hoof wall surface temperature (HWST) must remain below 10°C for the duration of the therapy. There are numerous methods available for the cooling of the digit. However, the most beneficial method available is a simple home-made technique. This involves immersing the hoof and distal limb into a bucket of ice and water, this will result in adequate HWST of below 5°C (Bamford 2019). This therapy should be performed for 20 minutes, every four hours to achieve adequate pain relief.
General nursing care
The pregnant mare may spend most of the time lying down due to pain. Decubital ulcers and muscle myopathies and neuropathies may develop. In recumbent animals, the veins and lymphatic vessels are easily compressed and may completely collapse, this is referred to as compartment syndrome (Dowling, 2019). To prevent this from occurring, thick bedding is necessary to reduce pressure on the underlying muscles. The bedding should range from six to 10 inches deep. It should be deep enough to throw yourself down on it and cushion your fall comfortably. The bedding must be compressible, comfortable and absorbent. Each time the horse is moved the bed should be aerated.
Decubital ulcers are difficult to minimise in a recumbent patient. They can be managed through optimal bedding and skin care. The most important factor is the bedding, it should be kept thoroughly dry and clean as wet skin is more prone to pressure sores and ulceration (Gardner 2011). Stable bandages can be applied to protect the distal limbs from self-trauma when getting up and down. Any shoes on the patient should be wrapped with tape to reduce the contusions/lacerations.
The mare should be groomed regularly and kept in good condition. These patients are used to human interaction and would benefit from a simple brush down. This could improve the patient’s mood, brighten their day and improve their mental state. Grooming can also aid in minimising the likelihood of pressure sores caused by excessive recumbency.
Pregnancy risks
A plan for parturition complications should be established for all laminitic mares. It's important to understand the complications that may arise and be prepared. Frequent observation is required, at least hourly, for evidence of early stage labour. Cameras placed in the stable are helpful aids for frequent check-ups on the mare. All equipment should be readily available beside the stable, ie. a foaling kit containing rectal sleeves, lubricant, foaling ropes, tail bandage, etc. A foetal resuscitation kit should also be on hand. A plan should be drawn up with regards to complications arising such as dystocia, should it occur, with permission for general anaesthesia and caesarean section obtained before the event so that time is not wasted (Wilkins, Acvim and Acvecc 2003).
Conclusion
In conclusion, the management of laminitis during pregnancy is challenging and may lead to severe lameness, insulin resistance, the birth of an abnormal foal, stillbirth, dystocia, future infertility or euthanasia. In severe laminitic cases, we may be unable to rehabilitate the horse to where it has an acceptable quality of life. Therefore, the prevention and treatment of laminitis at the developmental and acute phases are crucial. Pregnant mares appear to suffer from the development or aggravation of laminitis during gestation and can also be subjected to the disease after parturition. To achieve effective management and pain control it is important to incorporate optimal medical therapy, nutrition, hoof care and housing, rehabilitation, cryotherapy and general nursing techniques into a comprehensive patient care plan. Veterinary nurses have the responsibility to provide the best care for these patients, as their self-preservation is challenged.
Bassert J, Beal A and Samples O. Clinical Textbook for Veterinary Technicians. 9th ed. 2018. Missouri: Elsevier
Blanched T, Varner D, Schumacher J, Love C, Brinsko S & Rigby S. (2003). Manual of Equine Reproduction. 2nd ed. Philadelphia: Mosby 2003; 95-96
Bamford N. (2019). Clinical insights: Treatment of laminitis. Equine Veterinary Journal [online], 51. Available from: https://vimeo.com/313793857 [accessed 19 February 2019]
Canisso I, Rodriguez J, Sanz M and Coutinho da Silva M. A Clinical Approach to the Diagnostic and Treatment of Retained Fetal Membranes with an Emphasis Placed on the Critically Ill Mare. Journal of Equine Veterinary Science [online], 2013; 33(7). Available from: https://www.sciencedirect.com/science/article/pii/S0737080612004856 [accessed 15 March 2019]
Davies Z. Introduction to Horse Nutrition. Oxford: Blackwell Publishing; 2009
Dowling D. Equine Anaesthesia [online], VETSS7004: Anaesthesia & Analgesia. Dundalk Institute of Technology, Department of Science 2019; Available from: https://2019-moodle.dkit.ie/mod/folder/view.php?id=66008 [accessed 16 March 2019]
El-Ashker M, El-Khodery S, Metwally N, Hussein H, El-Boshy M. Prognostic Significance of Oxidative Stress Markers in Colitis Associated with Phenylbutazone Administration in Draft Horses. Journal of Equine Veterinary Science [online] 2012; 32(3): 146-152. Available from: https://www.sciencedirect.com/science/article/pii/S0737080611004722 [accessed 20 July 2019]
Galantino-Homer H and Engiles J. Insulin resistance and laminitis in broodmares. Journal of Equine Veterinary Science [online] 2012; 32(10). Available from: https://www-sciencedirect-com.ucd.idm.oclc.org/science/article/pii/S0737080612007344 [accessed 15 March 2019]
Gardner R. Evaluation and Management of the Recumbent Adult Horse. Veterinary Clinics of North America: Equine Practice [online] 2011; 27(3). Available from: https://www.sciencedirect.com/science/article/pii/S0749073911000502 [accessed 16 March 2019].
Gleerup K. (2018). Assessing pain in horses. In Practice 2018; 40(10): 457-463
Johnson P, Messer N, Ganjam S and Wiedmeyer C. Pregnancy-Associated Laminitis in Mares. Journal of Equine Veterinary Science [online] 2009; 29(1). Available from: https://www.sciencedirect.com/science/article/pii/S0737080608003961?via%3Dihub [accessed 29 January 2019]
Gordon M, McKeever K, Betros C, Manso Filho H. Exercise-induced alterations in plasma concentrations of ghrelin, adiponectin, leptin, glucose, insulin, and cortisol in horses. The Veterinary Journal [online] 2007; 173(3): 532-540. Available from: https://www.sciencedirect.com/science/article/pii/S109002330600013X [accessed 20 July 2019].
McDonnell L. Laminitis in the horse: part I. Veterinary Ireland Journal [online] 2017; 7(6): 290-292
McDonnell L. Laminitis in the horse: part II. Veterinary Ireland Journal [online] 2017; 7(7): 342-345
O’Grady S. A Practical Approach to Managing Acute Laminitis. In: 2013 Proceedings of the American Association of Equine Practitioners – Focus Meeting on the Foot, USA [online] 2013; 41-49. Available from: http://www.ivis.org [accessed 29 January 2019]
Parks A. Acute and Chronic Laminitis – An Overview. In: 2009 Proceedings of the American Association of Equine Practitioners – Focus Meeting Focus on the Foot, Columbus, Ohio, USA [online] 2009; 132-139 Available from: https://www.ivis.org/proceedings/aaepfocus/2009/parks.pdf [accessed 29 January 2019].
Stashak T. Practical Guide to Lameness in Horses. Oxford: Blackwell Publishing 2006; 183-196.
Wrigley J. (2011). Home care nursing for the laminitic horse. Journal of Equine Veterinary Science [online], 31(10). Available from: https://www.sciencedirect.com/science/article/pii/S0737080611005727 [accessed 24 January 2019].